Title
Why
Continuous monitoring of correct performance of the total testing process (consisting of the pre-analytical stage, the analytical stage, and the post-analytical stage) of the laboratory helps you to identify potential errors quickly and is one of the most important activities to create continuous improvement.
In the right-hand column background information is provided on process improvement from the WHO Laboratory Quality Management System (LQMS) handbook.
What
Monitoring correct performance of each single step of the total testing process is not feasible. Instead, identify critical control points in this process. These are points that can serve as indicator for correct performance of the process. These indicators are called quality indicators.
An example of a quality indicator is "percentage of rejected samples". This indicator gives information on the performance of the total process of sample collection, transport and reception. A high level or increase in the percentage of rejected samples must be regarded as a nonconformity and an investigation must be started to identify what causes this nonconformity. Upon identification of the cause corrective actions must be formulated to resolve the problem. Preventive actions must also be formulated to minimize the risk that the same error will reoccur. These actions all lead to improvement of laboratory quality. Continuously monitoring quality indicators and resolving errors in the total testing process detected by these quality indicators facilitates continuous improvement of the laboratory.
To obtain an insight in what quality indicators are, how they are used and to help you select appropriate quality indicators for your laboratory, read the articles as listed below and as provided in the right-hand column. These articles present results of several laboratories that have already formulated quality indicators and have tested their feasibility in achieving continuous improvement. Permission to reproduce the papers was kindly provided by De Gruyter publishing.
Kirchner MJ, Funes VA et al. Quality indicators and specifications for key processes in clinical laboratories: a preliminary experience. Clin Chem Lab Med 2007;45(5):672-7.
Plebani M, Ceriotti F, Messeri G, Ottomano C, Pansini N, Bonini P. Laboratory network of excellence: enhancing patient safety and service effectiveness. Clin Chem Lab Med 2006;44(2):150-60.
Ricos C, Garcia-Victoria M, de la Fuente B. Quality indicators and specifications for the extra-analytical phases in clinical laboratory management. Clin Chem Lab Med 2004; 42(6): 578-82.
Ricos C, Biosca C, Ibarz M, Minchinela J, Llopis M, Perich C, et al. Quality indicators and specifications for strategic and support processes in laboratory medicine. Clin Chem Lab Med 2008;46(8):1189-94.
How & who
Quality Officer:
- Read the articles referred to above.
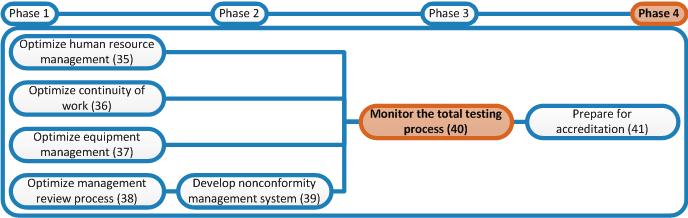
- Identify critical parameters of each process of your laboratory that can be used as quality indicator for this process. Use the flowcharts developed in phase 2 to help you identifying critical steps in each process and use the knowledge obtained from reading the articles referred to above.
- Start monitoring the quality indicators on a monthly basis. Insert data in Excel sheets. If a sudden change in the trends is seen for a specific indicator, complete a nonconformity form and follow the procedure described in the SOP for Nonconformity Management to identify the cause, resolve the nonconformity to get the value of the quality indicator down to its normal level and formulate preventive actions to prevent the same problem form reoccurring.
- When you have monitored the set of quality indicator for a certain amount of time (approximately 6 to 12 months), go one step further by setting a limit of acceptability for each indicator and trying to optimize laboratory processes such that you achieve these limits. E.g. if for the indicator "percentage of samples rejected" the value is normally around 5%, set the limit of acceptability on 3% sample rejection. Identify the causes leading most often to rejection of samples and try to resolve these causes. See if the percentage of rejected samples subsequently decreases. Repeat this process until the 3% limit is achieved. Setting limits of acceptability for each indicator and trying to optimize the laboratory processes such that their performance doesn't exceed these limits is called benchmarking. Try to minimize the limits of acceptability as much as possible to trigger maximum laboratory performance improvement. However, do not put pressure on the laboratory staff to achieve the benchmarks as it will then become a perverse activity that does more harm than good. The articles referred to above also provide information on use of quality indicators as benchmarks.