In Tanzania, the government and a range of stakeholders are collaborating to coordinate a national approach to collecting and analyzing data from health care facilities.
Without accurate data from health facilities, the government is unable to make informed decisions about how to improve the health system. A national coordinated approach is needed to reduce duplication and inefficiencies.
Improved data will lead to better decision-making, improved evidence-based policies, enhanced collaboration and standardized methods towards data analysis. This vitally contributes to progress towards UHC
The government is collaborating with WHO and other stakeholders to strengthen data governance. It is creating a national multi-programme health facility data system, applying the WHO standard data analysis package to explore further
Data represent what we do, and with data we are being held accountable, meaning we have to give weight to the way it is processed and reported.
This is one of the successes that we can proudly say: Tanzania has been able to bring together programmes to discuss common challenges so that we make the health system stronger together
Why does this matter?
Primary health care (PHC) is a core strategy for attaining universal health coverage (UHC) and data from primary care facilities plays a critical role. It’s a simple fact that without accurate data gathered and analysed from primary care facilities, governments are unable to make informed decisions about their health systems and make progress towards universal health coverage (UHC).
Important questions therefore need to be answered. How many people are visiting primary care facilities? What sort of health problems do they have? How are they being treated? How many are not seeking care? How many health workers with what skills are working in each clinic? How many medicines are available? Information about all these questions and more provide vital evidence to policy makers and managers so they can take the right decisions to improve primary health care, front line and hospital services and reach the ultimate goal UHC.
Everyone knows that data matters. The demand for data is growing, as countries are required to demonstrate their progress towards the Sustainable Development Goals (SDGs) or be accountable to development partners for specific programmes such as TB, malaria, vaccinations or maternal health. But this is where the data landscape gets very complex.
Multiple actors with overlapping activities in the health sector put huge demands for data on countries and health facilities. They require separate monitoring and evaluation plans, single-topic data collection systems and individual reports. Often, primary care facilities have to juggle the introduction of simultaneous but varied multiple digital innovations to collect and manage data, and struggle to harmonize disparate databases. Health sector data systems are buckling under the pressure. This piecemeal approach to PHC data, so crucial for decision-making to improve the population’s health, is ultimately failing the countries that donors are trying to support. Multiple and inharmonious efforts are never going to support a health system to grow stronger or help a country achieve UHC

Everyone knows that data matters. The demand for data is growing, as countries are required to demonstrate their progress towards the Sustainable Development Goals (SDGs) or be accountable to development partners for specific programmes such as TB, malaria, vaccinations or maternal health. But this is where the data landscape gets very complex.
Multiple actors with overlapping activities in the health sector put huge demands for data on countries and health facilities. They require separate monitoring and evaluation plans, single-topic data collection systems and individual reports. Often, primary care facilities have to juggle the introduction of simultaneous but varied multiple digital innovations to collect and manage data, and struggle to harmonize disparate databases. Health sector data systems are buckling under the pressure. This piecemeal approach to PHC data, so crucial for decision-making to improve the population’s health, is ultimately failing the countries that donors are trying to support. Multiple and inharmonious efforts are never going to support a health system to grow stronger or help a country achieve UHC
Tanzania’s data effort
The Government of Tanzania is committed to improving the quality of health data for evidence-based decision-making and wants to strengthen its capacity to track progress towards the health-related SDGs and UHC. Tanzania has taken major steps and made significant progress towards improving the
availability, access, analysis and use of primary care data, but now it also recognizes the need for more coordinated and collaborative efforts of all stakeholders to unleash the full potential of its health information system. This will reduce fragmentation and duplication of efforts, improve the efficiency of investments and build confidence in the national health data system.
Although Tanzania has faced multiple data challenges, the government through the Ministry of Health, has been consistent in showing leadership to coordinate with partners to improve the situation. On 11 September 2017, the Government launched the Tanzania Health Data Collaborative where partners and government can now hold joint discussions and make common investments in data systems. This is a collaboration of the Ministry of Health, Ministry of Community Development, Gender, Elderly and Children, the President’s Office Regional Administration and Local Government, health sector stakeholders, and global partners such as WHO.

"The Tanzania Health Data Collaborative will accelerate a series of joint priority actions to address gaps in our data and health information systems. Through our collaborative effort, we will have ONE platform that will allow us to collect all the information we need, be it information on what we do for HIV/AIDS interventions, for tuberculosis, for malaria, for reproductive and child health, or for maternal health.” said Dr Mpoki Ulisubisya,
The approach
Developing standards for PHC facility data systems that reflect current health service delivery and programmatic standards is crucial. This includes core indicators with standardized definitions (metadata), data quality assessment methods and best practice analytical methods and dashboards that can be applied systematically.
Standards are a foundation of quality as better data leads to better decisions, more effective actions and improved efficiencies; this is what drives better health systems and ultimately, UHC. WHO has published standards for PHC facility data analysis and use in the form of a toolkit with modules on mortality and morbidity, health services management, and programme-specific modules such as HIV, TB, malaria, maternal and child health, and immunization. Linked to each guidance module is a free downloadable digital package, that includes the core indicators and enables automated production of
standard dashboards. The digital packages can be used through any software platform.
There are four main areas to improve systematic data collection, analysis and use in PHC performance assessment and monitoring as part of progress towards UHC.
1. Address the gaps in analysis and use of data
Countries can refer to WHO modules to ensure that their existing PHC facility indicator sets, analysis
methods and ways of displaying and communicating data are in line with international standards and best practices. In practical terms, each programme needs to conduct a review exercise; and national and district planners and managers can use the relevant module to review or develop a crosscutting view of tracer indicators from multiple programmes. After review, the country’s electronic facility data system (for example the DHIS2) can be updated to reflect any changes.
To facilitate this, the country can install WHO’s electronic configuration packages. The installation process requires collaboration between programme data experts and information technology experts.
Once installed, the packages enable automated production of a key set of standard dashboards. This means that data users such as analysts, managers and policy makers across multiple levels and administrative areas of the country are able to view the data in a standard recommended way. (In the absence of such standardization, there is often a multiplicity of different charts and tables that may not reflect adequately the data needed for decision-making.) In addition, automation enables production of key analyses and visuals even in settings where data analysis capacity is limited; this also serves as a capacity-building mechanism for both data managers and health service managers
2. Promote systematic integrated approaches
All routine health facility data (from all programmes and all facility levels, especially PHC) should be available within a common, integrated electronic data system to allow decision-makers easy access to comprehensive health facility data and to enable use of relevant data across multiple programmes. Where this is not the case (for example where some programmes use independent systems), the various
systems should be interoperable. This means the various systems use standard data definitions (metadata) and data in one system can be accessed through another system. It is important for both ministries of health and donors or development partners to recognize the importance of this integrated approach to minimize the creation of multiple parallel systems that cannot “talk to each other”.

3. Support strong health information systems governance
All the components of a health information system – such as indicator selection, data collection tools and processes, reporting, data quality assurance, analysis, communication and use - rely on clear, standardized processes that are documented, endorsed and implemented. Staff members at all levels, especially primary care level, need to know their responsibilities and should have the capacities to carry them out. Non-existent or poorly implemented standard operational procedures have a negative impact on the availability of data and are frequently at the root of data quality problems.
4. Build networks of technical expertise
Well-functioning routine facility information systems need the combined efforts of several skill sets: clinical health care, public health, monitoring and evaluation, health management information systems and information technology. The WHO package of standards and best practices provides a foundation for common understanding and capacity building and it is important to develop country networks of data management practitioners and experts to share knowledge and lessons learned. Importantly, this includes those working at primary care level.
Health data system
The government of Tanzania is now a pioneer in promoting common agreements among national and international partners and finding a common agenda to improve the PHC health data system. Tanzania wants to have more streamlined data governance, compatibility among all health data systems, capacity to use these systems properly, ability to use the data collected and common investments in digital innovations.
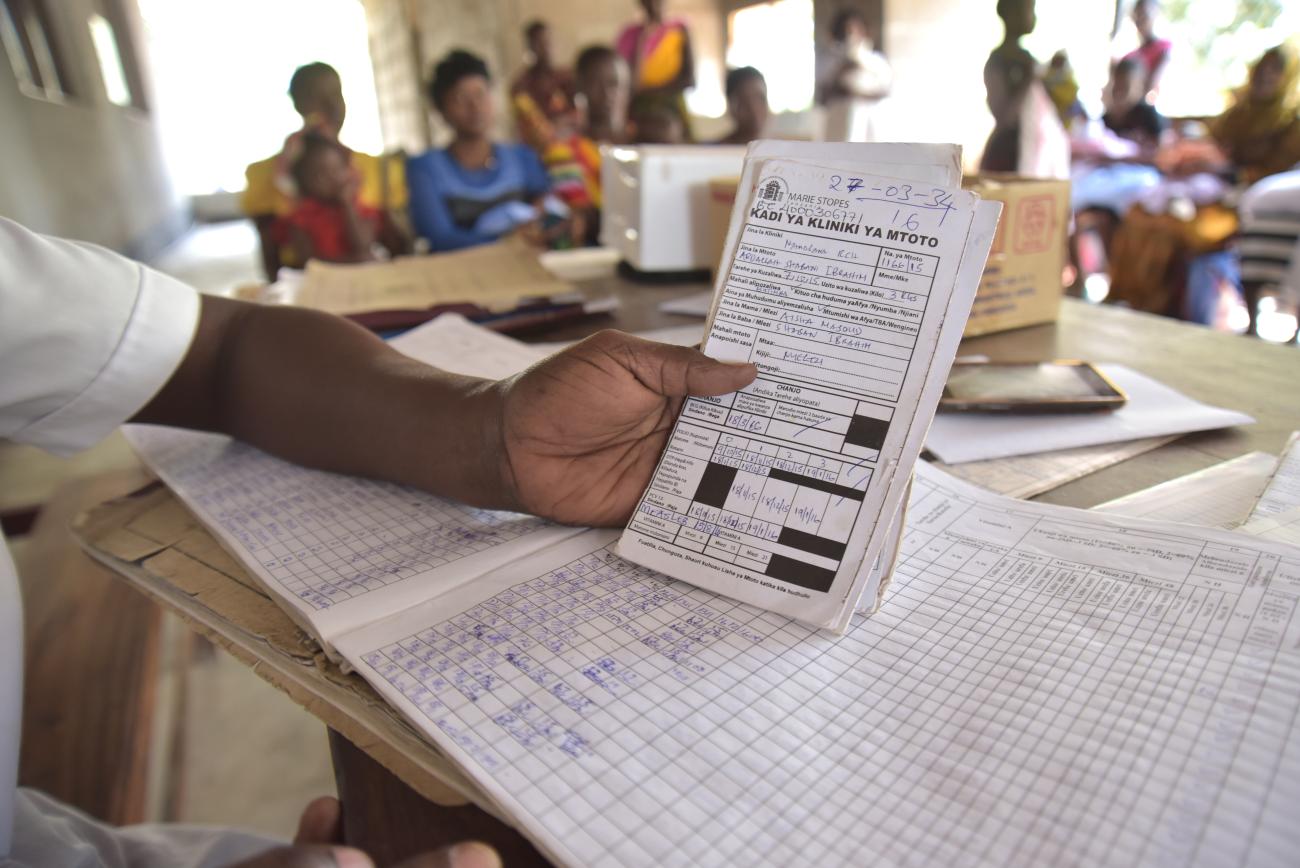
Particularly concerned with multiple data systems, the Ministry of Health drew up a concept note to introduce a national multi-programme health facility data system. In January 2019, the Ministry of Health invited country and external partners to its own multi-programme data workshop with over 70 national data specialists and programme specialists from TB, malaria, HIV, immunization and maternal and child health. The idea was to ensure that everyone was addressing common issues using common methods to promote integrated data approaches across in the health system.
Over three days, participants learned about the WHO standard data analysis package, and teams working in their specific programme areas looked into their own data sets and dashboards. Each team was able to identify challenges and successes and critique the standard databases developed by WHO. They highlighted recommendations that would help the health system move forward in areas of data, evidence generation and decision-making. The workshop facilitated mutual learning and ideas around how to share resources across programmes
"When we convened to listen to all the challenges and successes that each programme team faced, a surprising factor is that most of the challenges were common; we had just never had a forum to discuss them. This is one of the successes that we can proudly say: Tanzania has been able to bring together programmes to discuss common challenges so that we make the health system stronger together,” said Irene Mwoga, Strategic Information Systems Officer, WHO.
Following the multi-programme data workshop, some of the programmes are already working towards the recommendations made. In Human Resources for Health (HRH) experts in health systems, HRH and programmes are now coming together to find a common way forward to generate data that can inform policy decisions.
As Tanzania takes this health data system forward, the benefits are clear: improved data at PHC level will lead to better decision-making, improved evidence-based policies, enhanced collaboration, and standardized methods towards data analysis. All this makes a vital contribution to ensuring that the population has access to quality primary health care services, and therefore that Tanzania makes meaningful progress to UHC.