Mongolia is reaching remote populations and ensuring they can all receive good quality and affordable services by introducing a mobile people-centred integrated primary health care approach.
Mongolia has a vast land area, so ‘leaving no one behind’, means adapting mobile health services and technologies to get to those who are otherwise hard to reach.
Nomadic populations can access integrated health services, receive health promotion interventions, early diagnosis and treatment of diseases in time for them to have a positive impact.
WHO, through the UHC Partnership, has supported the strengthening of primary health care and the health system backed by adequate funding, strong health plans and evidence-based policies.

"Expanding use of mobile health technology at PHC has resulted in the M-Health initiative being a key component for outreach services during COVID-19 ensuring that services reach the unreached at national and subnational levels of the health system."

"The Government of Mongolia has committed to making PHC more responsive and equitable to the needs of the population. I would like to note that measures, taken by Ministry of Health with support of World Health Organization bring significant progress in the health sector towards achieving UHC."

“Thanks to WHO’s continued support to prepare, strengthen multi-sectoral information sharing, management of resources, and workforce development, we didn’t have any local transmission of COVID-19 until 11 November 2020.”

"Thanks to the M-Health initiative, the quality and access to preventive health examinations among local people has improved in the last two years. In 2019, coverage of preventive health examinations reached 90% of the population. Most remote herders live 130 kilometres away from the soum [sub-province] health centre and health workers mainly reached them through the mobile health service delivery."
THE LONG READ
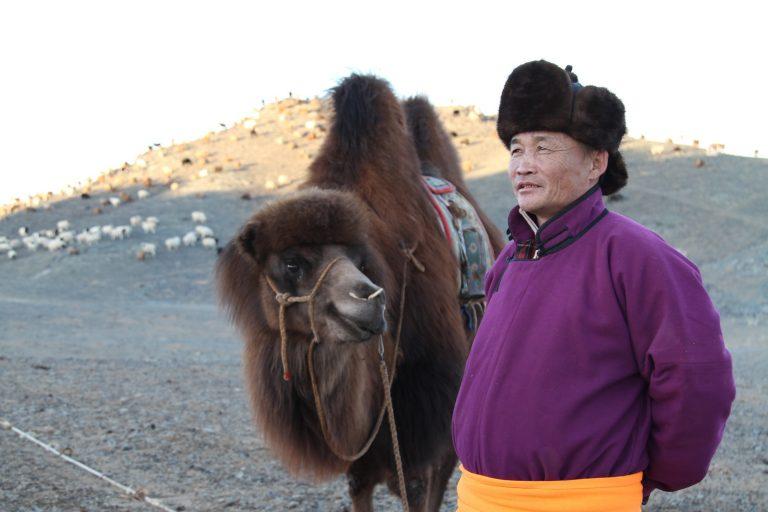
Norov Bayarjargal, a local herder in the Gobi Desert, stands in front of a makeshift mobile health clinic in Dersene-Us, his native village in the southern tip of Mongolia. Beside him are two yurts and occasional herds grazing the land, but in the distance there is nothing but desert and sky for miles. Norov has just had a consultation with a mobile health team from the sub-provincial health centre, which visits herder communities in their own homes.
The mobile health team screens herders and their families for communicable and non-communicable diseases, signs of cholesterol and sugar in their blood and they offer ultrasounds for women. One month ago, through this service, Norov was diagnosed with gallbladder and kidney problems and was referred to the nearest local (sub-province or soum) health centre, where a specialist gave him the medicines he needed.
“Because of the mobile health screening, I was diagnosed early and received timely treatment. The health professionals advised me to cut down my salt and animal fat intake. I know that health is wealth and that I need to make healthy living choices now, irrespective of financial challenges,” said Norov.

With a vast land area, Mongolia faces many challenges in delivering health services to its citizens especially those living in disadvantaged and remote rural areas, including vulnerable and nomadic populations, migrants and unregistered people.
From 2016-2020, the government operated an initiative called: ‘Expanding use of mobile health technology in primary health care towards universal health coverage in Mongolia’ or M-Health. It was supported by WHO, through the UHC Partnership and the Korea Foundation for International Health Care and Community Chest of Korea.

Primary health care providers are also noticing the difference that the M-Health initiative is making to the lives of remote populations.
“Thanks to the M-Health initiative, the quality and access to preventive health examinations among local people has improved in the last two years. In 2019, coverage of preventive health examinations reached 90% of the population. Most remote herders live 130 kilometres away from the soum [sub-province] health centre and health workers mainly reached them through the mobile health service delivery,” said Dr Chuluuntsetsetseg Erdenechuluun, Head of the Mandakh Soum Health Center, Dornogobi Province.
Mongolia is among the 115 countries and areas to which the UHC Partnership helps deliver WHO support and technical expertise in advancing UHC. The Partnership is funded by the European Union (EU), the Grand Duchy of Luxembourg, Irish Aid, the Government of Japan, the French Ministry for Europe and Foreign Affairs, the United Kingdom – Foreign, Commonwealth & Development Office and Belgium.

Laying the foundations for equity
All the lowest administrative units in Mongolia have primary health care (PHC) facilities, making health services geographically, financially and administratively accessible. But there are challenges. Although Mongolia has 7,500 PHC providers who are working at 536 facilities, use of these local services is not optimal as communities tend to bypass them to access secondary or tertiary level care. The ongoing problem threatened to become more acute when COVID-19 arrived.
Recent investments in PHC for UHC, such as increasing the budget, introducing Social Health Insurance (SHI) financing for extending the PHC service package served as a critical foundation for the health system, allowing it to adapt to the pandemic scenario. The principle of equity, or the ambition to ‘leave no one behind’, was the driver to deliver PHC services to the most disadvantaged, hard-to-reach populations in Mongolia. In times of COVID-19, reaching remote populations with the same level of engagement and communication as the rest of the country is vital.
WHO, through the UHC Partnership, has been working closely with the government since 2018 to strengthen PHC strategic financing and improve quality of care. This previous work has also been fundamental in laying the foundations for a stronger national response to COVID-19.

Reaching remote groups through mobile health
Herders, due to their remote settings and lifestyles, are often unable to visit a soum or sub-province health centre. They are grateful that early diagnoses of diseases and subsequent consultations are available locally and that they have further examinations once a year, when needed.
“I was very appreciative that herders like me got screened for diseases at home, and I did not have to travel a long distance to get medical services,” said a herder from Adaatsag Soum, Dornogobi Province.
“I was wondering why medical people came to my home, and then they explained it was for us to undergo for preventive ultrasound and ECG examinations. I was surprised that medical equipment had become such a small size,” said another herder from Shiveegobi Soum, Gobisumber Province.


The Mongolian State Policy on Health (2017-2026) identifies the “need to expand the use of mobile service and technologies at the primary health care level to better reach out to target groups such as people in remote areas and the poor and vulnerable populations”.
The M-Health initiative is now being implemented in 21 provinces across Mongolia and 9 districts in Ulaanbaatar City. Bringing the initiative to urban areas is helping migrants from rural to urban areas who have lost their herds and livelihoods, and are particularly vulnerable. People of all ages, including older people, children and adolescents are able to access M-Health services, especially those living in remote rural and urban areas.
As part of the initiative, PHC providers conduct integrated health services through three types of service delivery: home visits, mobile health services combined with home visits and health centre services. All these include health examinations, screening and health promotion activities related to maternal and child health, communicable diseases and non-communicable diseases. Mobile health services, in combination with home visits, are mostly used to reach disadvantaged communities, including herders, migrants, and low-income groups.

At the request of the Ministry of Health and local health organizations, WHO also supporting capacity building for integrated PHC service delivery so that patients get the quality people-centred care throughout their life-course, including prevention, treatment, rehabilitation and palliative care.
The Government of Mongolia, along with local governments, recognized the value and cost-effectiveness of reaching remote and disadvantaged populations. As a result, since 2016, this initiative has been expanded to another 121 local areas supported mostly by local governments and a few of them supported by development partners and private companies. In 2021, in order to maintain essential health services during the COVID-19 pandemic and beyond, WHO has been continuously providing support in other 63 remote areas.
“Expanding use of mobile health technology at PHC has resulted in the M-Health initiative being a key component for outreach services during COVID-19 ensuring that services reach the unreached at national and subnational levels of the health system, ” said Dr Sergey Diorditsa, WHO Representative to Mongolia.

The M-Health initiative also contributes to stronger coordination, collaboration and integration of the various work programmes within WHO Mongolia and with various partners including the Ministry of Health, development partners, donors and other key stakeholders.
“The Government of Mongolia has committed to making PHC more responsive and equitable to the needs of the population. I would like to note that measures, taken by Ministry of Health with support of World Health Organization bring significant progress in the health sector towards achieving UHC,” said Dr Sereejav Enkhbold, Minister of Health, Mongolia.

Responding to COVID-19
On 11 November 2020, the first local case of COVID-19 was confirmed in Mongolia and numbers reached 4,073 within four months. Compared to other countries around the region, Mongolia has had relatively low number of cases, with four reported deaths as of 18 March 2021. In order to prevent the virus from spreading, the government focused on risk communication and community engagement. COVID-19 has been a litmus test to the readiness of Mongolia’s emergency response built over the last decade.
Based on lessons learned from SARS and H1N1, a multi-sectoral coordination and communication system was established for all types of emergencies. The foundation of Mongolia’s strategy for COVID-19 has been solidarity, early preventative measures, strong coordination and partnership and a culture of continuous improvement.
Over the past years, Mongolia has demonstrated its commitment to strengthening and improving its pandemic preparedness efforts. Pandemic preparedness planning in Mongolia has been integrated into national and local general disaster management planning, processes and structures. Plans and processes have involved multiple sectors, civil society, NGOs, private sector and health cluster partners. In 2017, the country volunteered for a Joint External Evaluation (JEE) of its capacities to prevent, detect and respond to health emergencies. A formal coordination system for preparedness and response to all types of public health events and emergencies was established in 2017. Since 2016 Mongolia has completed six Simulation Exercises (SimEx) to further develop, assess and test the functional capabilities of its emergency systems, procedures and mechanisms to be able to respond to outbreaks or public health emergencies, such as COVID-19.
“Thanks to WHO’s continued support to prepare, strengthen multi-sectoral information sharing, management of resources, and workforce development, we didn’t have any local transmission of COVID-19 until 11 November 2020,” said Sayanaa Lkhagvasuren, Advisor on COVID-19 prevention to Mongolia’s Deputy Prime Minister.

Primary health care and universal health coverage
Many health issues, as well as COVID-19, have the gravest impact on people who are socially, economically or geographically disadvantaged. Addressing equity and reaching those most in need of health services requires a strong focus on PHC for UHC, as a response to current and future health challenges. The UHC Partnership will continue to support the government with the expansion of telemedicine, mobile services and mobile and portable technologies at the PHC level, including rapid COVID-19 tests as a cost-effective measure. The Partnership will also support the strengthening of multisectoral collaboration to address health for all policies.