Our website has moved!
The WHO Centre for Health Development (WHO Kobe Centre – WKC) has changed its website location to a new, simple web address: https://wkc.who.int/
We will no longer be updating the current website (https://extranet.who.int/kobe_centre/en), and no new content will be uploaded here. Visitors to this old site will still be able to see old content until the middle of December, after which it will be archived.
Please go to https://wkc.who.int/ to see all the new, improved features and see how easy it is to navigate the site. We hope you will visit us soon!

2023 UHC Day Message of Dr Sarah Barber, Director, WHO Centre for Health Development
On 12 December, Universal Health Coverage (UHC) day, we at the WHO Centre for Health Development (WHO Kobe Centre - WKC) are encouraged by the renewed commitment of the global community to achieving UHC for all, arising from the United Nations Political Declaration on UHC in New York on 21 September 2023.
With the theme this year being “Health for All: Time for Action”, WKC affirms that UHC is central to achieving all of the Sustainable Development Goals (SDGs).
Health service coverage and financial protection are two key indicators that measure progress on UHC. WKC’s research on unmet needs, particularly of older populations, contributed to the 2023 WHO-World Bank Global Monitoring Report on UHC, and informed discussions at the United Nations High-Level Meeting on UHC in September 2023.
Financing UHC is an investment, not a cost. Importantly, improving the quality of care for people with chronic conditions is key to reducing preventable deaths and advancing UHC. With rapid population ageing, changes are needed in how to pay for chronic care that provides incentives for quality.
Our work on the WHO Flagship Project with partners at WHO Headquarters and the OECD on purchasing arrangements to strengthen quality care for chronic diseases explored whether different types of payment arrangements incentivised healthcare providers to provide better quality care for chronic conditions.
While rigorous evaluations of effectiveness are still lacking, case studies in eight countries* found what facilitated the delivery of quality chronic care included health information systems and technology, strong leadership and multistakeholder engagement. Our evidence shows there should be a stronger focus on healthcare delivery models and how payments can support changes in service delivery mechanisms to improve quality.
This UHC Day, we join with millions around the world in urging leaders to make smarter investments in health to move the world closer to UHC by 2030 and deliver health for all. The consequences of underinvesting in UHC are unaffordable.
*For more information, see the case studies on Australia, Canada, Chile, China, Germany, Indonesia, South Africa and Spain.
Systematic review of effective health system responses for the prevention and control of non-communicable diseases in ASIA
Background
Health systems across high-, middle-, and low-income countries are facing challenges due to the increasing burden of non-communicable diseases and aging population (1). Lack of financial protection, limited access to essential drugs, shortages of trained health workers, and provision of continuous care for chronic conditions are some of the challenges facing health systems for managing chronic care (1). Some aspects of successful health systems include experimentation, appropriate selection of strategies and learning from other countries (2). Japan has succeeded in reducing mortality from chronic conditions, e.g., stroke and ischemic heart disease, through strengthening their primary health system. These public health efforts have contributed to increases in life expectancy since the 1960s (3). This study reviews the key interventions and tools to enhance the performance of health systems in selected countries in Asia.
Goal
The goal of this research is to review the cost-effectiveness of existing programmes and policies to strengthen health systems for chronic disease prevention and control. The review addressed the following research questions:
- Does any community intervention or health promotion activity for the prevention of diabetes, obesity, dyslipidemia or hypertension reduce cardiovascular events and mortality in East or Southeast Asian countries ?
- Is there any cost-effective community intervention or health promotion activity for the prevention of diabetes, obesity, dyslipidemia or hypertension in East or Southeast Asian countries?
Methods
This is a systematic review of peer-reviewed published randomized controlled trials (RCTs) and quasi experimental studies on the prevention and control of NCDs in Asian countries. MEDLINE, the Cochrane Library and Ichushi were systematically searched for all available years using key words and subject headings. Full articles, in English and Japanese languages, reporting the effects of community intervention or health promotion on cardiovascular events (e.g. stroke; myocardial infarction) and overall mortality and/or reporting the cost effectiveness of these interventions were included in this study. Studies were excluded if they only had an abstract, were reviews, development, usability, or feasibility studies, had a non-Asian sample, described a hospital-based intervention or an intervention for which the end users were not patients with NCDs.
Results
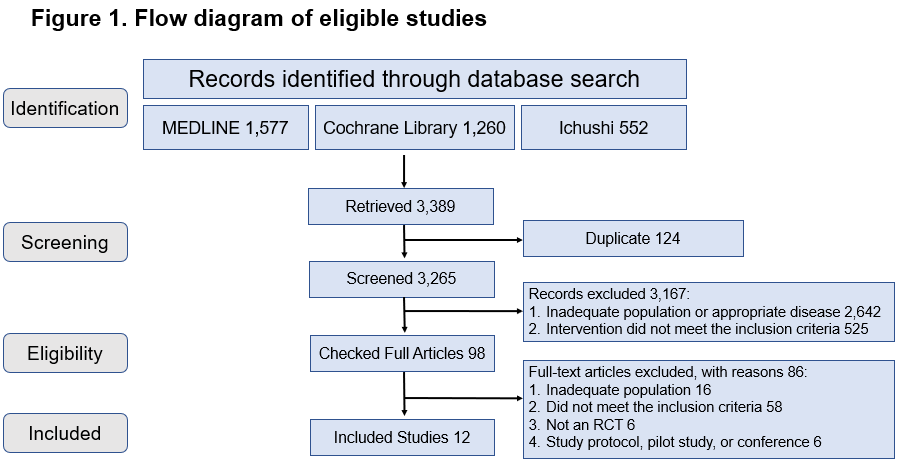
The flow diagram of eligible studies is shown in figure 1. Out of 3389 studies, only twelve full-text articles met all inclusion and exclusion criteria. Three papers were from Japan, seven from China/Hongkong SAR, and two studies were from South Korea. Four papers examined the effect of community intervention or health promotion on the incidence of cardiovascular events or mortality. The duration of interventions ranged from 21.5 months to 15 years, and targeted population with hypertension, diabetes, impaired glucose intolerance or obesity. Overall, the interventions were effective in reducing the incidence of stroke, cardiovascular disease mortality, or all-cause mortality depending on the studies. Eight studies examined the cost effectiveness of interventions on hypertension, diabetes, and obesity. The studies were generally found to be cost-effective, despite heterogeneity by types of outcomes and method of assessments.
Implications
The review revealed a significant lack of research on the effects of community intervention and health promotion on the incidence of cardiovascular events and mortality among individuals with underlying NCDs and NCD risk factors in East and Southeast Asia. This limits the potential to derive meaningful and evidence-based policy recommendations.
References
1. Hunter DJ, Reddy KS. Noncommunicable Diseases. New England Journal of Medicine. 2013;369(14):1336-43. doi: 10.1056/NEJMra1109345.
2. Balabanova D, Mills A, Conteh, et al. Good Health at Low Cost 25 years on: lessons for the future of health systems strenghening. Lancet. 2013;381:2118-33.
3. Ikeda N, Saito E, Kondo N, et al. What has made the population of Japan healthy?. Lancet. 2011;378:1094-105.

Mapping service delivery models that optimize quality of life and health services use among older people
Background
As populations age, health and social services need to be realigned towards older populations to optimize their functioning and quality of life (QOL). This requires fundamental changes to health systems and service delivery to meet the needs of older people and achieve intended outcomes, particularly for those with advancing chronic disease.
Phase 1: In 2017, researchers completed a rapid review of systematic reviews on the effectiveness of service models aiming to optimize QOL for older people. Of 2238 identified, 72 systematic reviews were retained. Service models broadly classified as to whether they targeting physical functioning or focused on symptoms. However, the study could not draw conclusions about which service delivery model contributed to specific outcomes, nor could it describe which models would work in resource constrained settings in low and middle-income countries (LMIC).
Phase 2: To address the gaps in Phase 1, undertake a tertiary review of primary literature to map service delivery models to specific outcomes that optimize both quality of life and health services use for older people, and describe the elements that are needed for the models to work in other contexts.
Phase 2 Methods
To analyze the primary studies identified from the original scoping review and evaluate linkages between service delivery models, their elements, organization and delivery to describe how intended outcomes for older populations.
Findings
Common elements of services that optimize quality of life and health service use in older people include a comprehensive and ongoing assessment of needs and sufficient time for this to occur. Enabling factors include patient engagement, participation and self-management.
Facilitating health systems factors including skilled workforce, systems that enable interdisciplinary coordination, referral systems to enable access to specialized care, and family support systems.
The study failed to draw associations between the health systems elements and health outcomes or care utilization.
The study noted that there was insufficient evidence to assess the impact of bereavement support for carers, integration of health and social care, and the use of volunteers and community-based organisations.