Systematic review of effective health system responses for the prevention and control of non-communicable diseases in ASIA
Background
Health systems across high-, middle-, and low-income countries are facing challenges due to the increasing burden of non-communicable diseases and aging population (1). Lack of financial protection, limited access to essential drugs, shortages of trained health workers, and provision of continuous care for chronic conditions are some of the challenges facing health systems for managing chronic care (1). Some aspects of successful health systems include experimentation, appropriate selection of strategies and learning from other countries (2). Japan has succeeded in reducing mortality from chronic conditions, e.g., stroke and ischemic heart disease, through strengthening their primary health system. These public health efforts have contributed to increases in life expectancy since the 1960s (3). This study reviews the key interventions and tools to enhance the performance of health systems in selected countries in Asia.
Goal
The goal of this research is to review the cost-effectiveness of existing programmes and policies to strengthen health systems for chronic disease prevention and control. The review addressed the following research questions:
- Does any community intervention or health promotion activity for the prevention of diabetes, obesity, dyslipidemia or hypertension reduce cardiovascular events and mortality in East or Southeast Asian countries ?
- Is there any cost-effective community intervention or health promotion activity for the prevention of diabetes, obesity, dyslipidemia or hypertension in East or Southeast Asian countries?
Methods
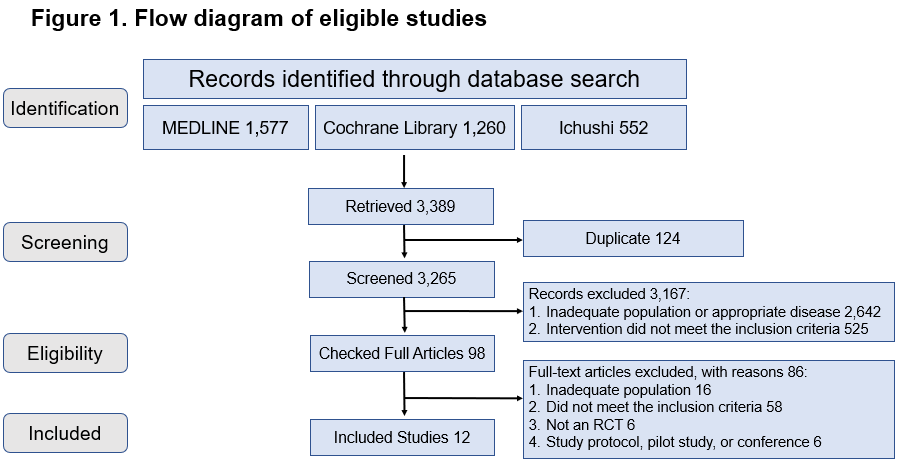
This is a systematic review of peer-reviewed published randomized controlled trials (RCTs) and quasi experimental studies on the prevention and control of NCDs in Asian countries. MEDLINE, the Cochrane Library and Ichushi were systematically searched for all available years using key words and subject headings. Full articles, in English and Japanese languages, reporting the effects of community intervention or health promotion on cardiovascular events (e.g. stroke; myocardial infarction) and overall mortality and/or reporting the cost effectiveness of these interventions were included in this study. Studies were excluded if they only had an abstract, were reviews, development, usability, or feasibility studies, had a non-Asian sample, described a hospital-based intervention or an intervention for which the end users were not patients with NCDs.
Results
The flow diagram of eligible studies is shown in figure 1. Out of 3389 studies, only twelve full-text articles met all inclusion and exclusion criteria. Three papers were from Japan, seven from China/Hongkong SAR, and two studies were from South Korea. Four papers examined the effect of community intervention or health promotion on the incidence of cardiovascular events or mortality. The duration of interventions ranged from 21.5 months to 15 years, and targeted population with hypertension, diabetes, impaired glucose intolerance or obesity. Overall, the interventions were effective in reducing the incidence of stroke, cardiovascular disease mortality, or all-cause mortality depending on the studies. Eight studies examined the cost effectiveness of interventions on hypertension, diabetes, and obesity. The studies were generally found to be cost-effective, despite heterogeneity by types of outcomes and method of assessments.
Implications
The review revealed a significant lack of research on the effects of community intervention and health promotion on the incidence of cardiovascular events and mortality among individuals with underlying NCDs and NCD risk factors in East and Southeast Asia. This limits the potential to derive meaningful and evidence-based policy recommendations.
References
1. Hunter DJ, Reddy KS. Noncommunicable Diseases. New England Journal of Medicine. 2013;369(14):1336-43. doi: 10.1056/NEJMra1109345.
2. Balabanova D, Mills A, Conteh, et al. Good Health at Low Cost 25 years on: lessons for the future of health systems strenghening. Lancet. 2013;381:2118-33.
3. Ikeda N, Saito E, Kondo N, et al. What has made the population of Japan healthy?. Lancet. 2011;378:1094-105.

Mapping service delivery models that optimize quality of life and health services use among older people
Background
As populations age, health and social services need to be realigned towards older populations to optimize their functioning and quality of life (QOL). This requires fundamental changes to health systems and service delivery to meet the needs of older people and achieve intended outcomes, particularly for those with advancing chronic disease.
Phase 1: In 2017, researchers completed a rapid review of systematic reviews on the effectiveness of service models aiming to optimize QOL for older people. Of 2238 identified, 72 systematic reviews were retained. Service models broadly classified as to whether they targeting physical functioning or focused on symptoms. However, the study could not draw conclusions about which service delivery model contributed to specific outcomes, nor could it describe which models would work in resource constrained settings in low and middle-income countries (LMIC).
Phase 2: To address the gaps in Phase 1, undertake a tertiary review of primary literature to map service delivery models to specific outcomes that optimize both quality of life and health services use for older people, and describe the elements that are needed for the models to work in other contexts.
Phase 2 Methods
To analyze the primary studies identified from the original scoping review and evaluate linkages between service delivery models, their elements, organization and delivery to describe how intended outcomes for older populations.
Findings
Common elements of services that optimize quality of life and health service use in older people include a comprehensive and ongoing assessment of needs and sufficient time for this to occur. Enabling factors include patient engagement, participation and self-management.
Facilitating health systems factors including skilled workforce, systems that enable interdisciplinary coordination, referral systems to enable access to specialized care, and family support systems.
The study failed to draw associations between the health systems elements and health outcomes or care utilization.
The study noted that there was insufficient evidence to assess the impact of bereavement support for carers, integration of health and social care, and the use of volunteers and community-based organisations.

Community based social innovations for healthy communities in Japan
Background
Ensuring fiscal and financial sustainability of the health and social care system is regarded as an important policy goal. In several high-income settings, such as Canada, Japan, Norway, Sweden and Switzerland, there is a preference for staying in communities as one ages rather than institutional care. This has resulted in greater numbers of older persons living in the community. This trend requires different arrangements and social networks to care for the needs of older people.
Community-based social innovations (CBSIs) are one type of innovation that may help to address the needs of older people. Previous research and consultations have defined the principles underlying CBSIs: the empowerment of older people to care for themselves, social inclusion, and maintaining wellbeing. This project explores the context of CBSIs in Japan, where the population has the highest life expectancy globally, and the population of 85 years and older is increasing.
Goal
To provide a better understanding of community-based social innovations in Japan, their scope, how they connect health and social services, and community impact.
Methods
-
Participant observation at three communities in Northern Hyogo Prefecture, including one urban programme, one farming and one fishing community.
-
Ten in-depth qualitative semi-structured interviews with local government officials and community leaders and three focus group discussions with community members.
-
Analysis was done using the Grounded Theory approach.
ICF-based assessment tool development for care skill training in Japanese long-term care system
Background
With growing numbers of people living with disability and chronic morbidities, more long-term care professionals are needed to ensure access to quality, cost-effective services. East Asia is already facing a serious shortage of care workers], while in Japan, an additional 380,000 care workers will be needed by 2025 when the post war baby boomers will be 75 years or older. To respond to this growing need, countries are increasing the recruitment and/or training of foreign health workers. For example, in Canada and the United States, foreign health workers represent around one-fifth of the total long-term care workforce.
Japan has received foreign nurses and care workers from Indonesia, the Philippines and Vietnam as part of the Economic Partnership Programme. Recently, the country expanded its Technical Intern Training Programme to include training of foreign health care workers wishing to work in the health care industry in Japan, and exporting Japanese experiences in the field of continuing care as part of its international cooperation programme. With the growth of foreign workers in health care, it is crucial to ensure that training programmes effectively transfer care skills to trainees.
Goal
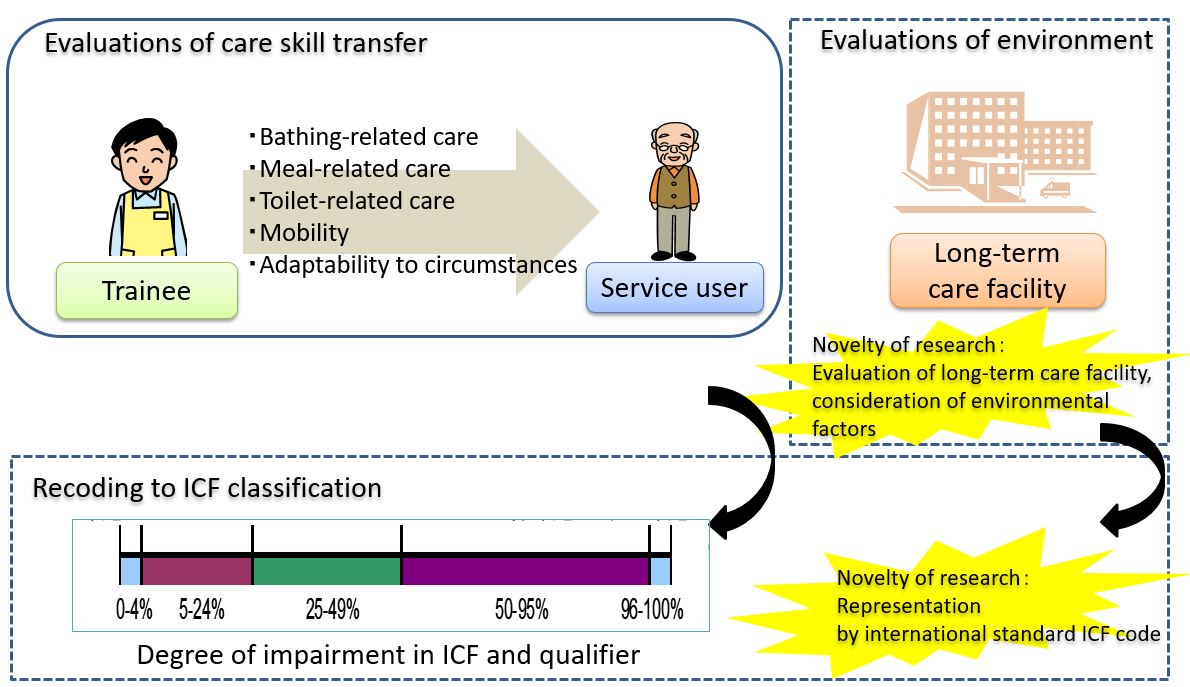
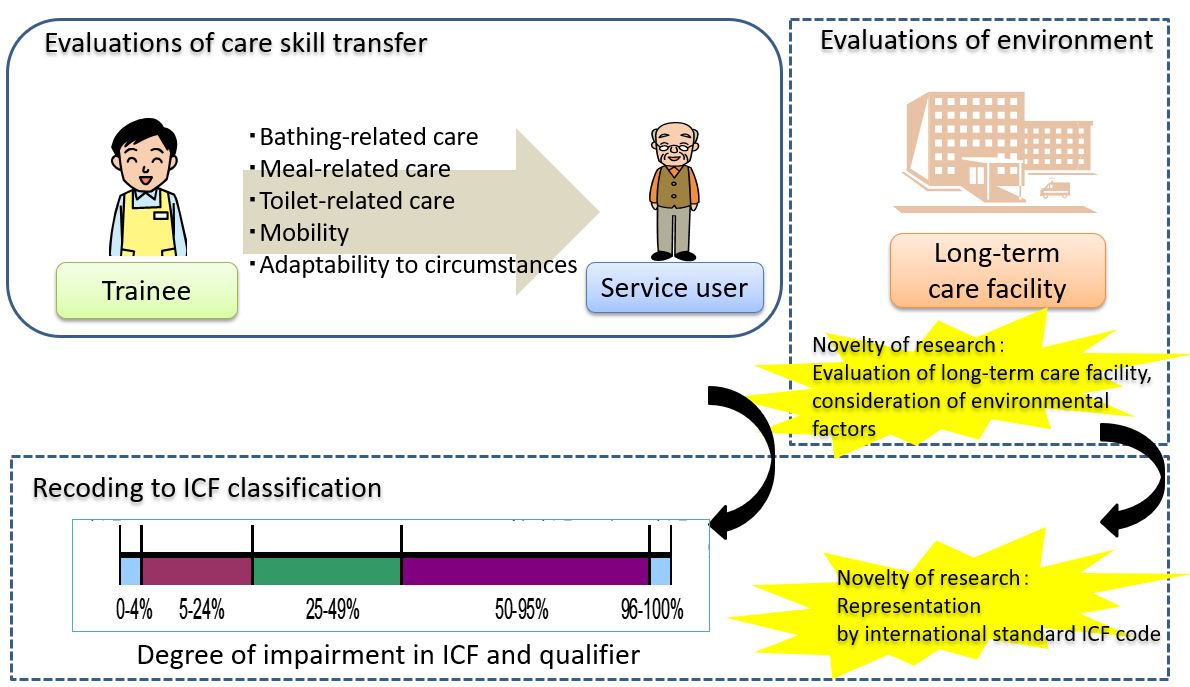
To develop and validate an evaluation tool based on the International Classification of Functioning, Disability and Health (ICF) to assess the transfer of health care skills in Japan’s Technical Intern Training Programme.
Methods
The new evaluation tool built on existing assessment tools of the Technical Intern Training Programme to incorporate the ICF, and was developed with inputs from a practitioners’ committee of nurses and doctors.
It was pre-tested in selected facilities involved in the Technical Intern Training Programme to identify potential difficulties around comprehension and administration of the evaluation instrument, and to modify the tool accordingly. The tool collected information on the care skill of the trainee, the care requirement of the care receiver, the background of the technical intern, and the employment environment.
The evaluation of whether the care skills had been acquired at the end of the training was determined qualitatively with a sample of trainers. In addition, semi-structured interviews were conducted with facility managers, trainers and foreign trainees for qualitative feedback.
Results
The evaluation tool was field tested in 100 facilities on 300 trainers of foreign technical interns. Most trainers and staff indicated that 38 items covering the four elements of the care skill training system were difficult to use and recommended downsizing the evaluation tool to a maximum of 25 items. Participants suggested a guidebook to clarify the concepts of the ICF and its relevance to the grading of care competencies. Moreover, the heterogeneities in the baseline skill level between the trainees imply that the tool should be sensitive to capture the nuances of how progress is measured from different baseline levels.
Implications
The current project has produced an ICF-based evaluation tool to assess health care skills transfer within Japan’s Technical Intern Training Programme. Since it draws upon the constructs of the WHO ICF, this new tool can potentially be used in other international settings, particularly by countries wishing to employ foreign health care workers. The outcome of this project could have far-reaching implications as the need for health care for older persons, and the reliance on foreign workforce continues to grow, particularly in countries with rapidly ageing populations.

Evidence for improving health care provision to ensure universal health coverage amid rapid population ageing in Japan
Background
Health systems in resource-constrained and rich countries face continued challenges due to increasing population ageing and chronic morbidities. Conditions such as hip fractures and dementia are on the rise and their careful assessment could provide insights into the performance of health systems around access to and equity of health care. Big data in health care can assist to understand patterns of population health and to draw on relevant policies to improve health care and equity. Japan has made tremendous efforts to build large-scale health care databases through relevant laws or other mechanisms. These include for example the Diagnosis Procedure Combination (DPC) database, the National Receipt Database, the Comprehensive Long-Term Care Insurance database, and Adverse Reaction report database. However, the use of these databases to inform policies towards provision of equitable, cost effective, and quality health care services is very limited. This project involved several studies relating to the use of large-scale health care databases to address the growing concerns of equity in access to health care associated with population ageing in Japan. This research brief provides highlights from one of those studies which was based on an analysis of the DPC database, a health care insurance claims database.
Methods
The study involved a cross-sectional, secondary data analysis of the DPC database. The database consists of patients’ socio-demographic profile; principal diagnoses; comorbidities at admission; complication after admission; and procedures including surgery, medications and devices during hospitalization; length of stay; discharge status; and medical expense. The target population was patients aged at least 65 years with a diagnosis of a closed hip fracture during the study period (April 2014 – March 2018). The outcome variables were: receipt of surgical treatment for hip fracture and number of waiting days until surgery. The main explanatory variable of interest was dementia status. The analyses were adjusted for age, sex, fracture type, comorbidities, coma/consciousness level, ambulance use, as well as hospital characteristics, through multilevel analysis.
Results
The analytical sample consisted of 214,601 patients with first-time diagnosis of hip fracture, of which 58,400 (27.2%) had mild dementia, 44,787 (20.9%) had severe dementia and 159,173 (74.2%) received hip surgery. The mean number of waiting days before surgery was 3.66 days (± 3.72 days). Patients with severe dementia were more likely to receive hip surgery and more likely to experience a shorter waiting time until surgery compared to those without dementia. Older patients were less likely to receive surgery (80 years and above versus 65-79 years) but experienced a shorter waiting time before surgery (90 years and above versus 65-79 years).
Implications
This study has demonstrated the usefulness of employing large-scale data to address key questions in health care and equity. In contrast to the general trend that patients with psychiatric illness have less access to health care, this study revealed that patients with dementia in Japan may be prioritized for hip surgery. This approach should be considered in Japan and elsewhere in the region to address other relevant health care issues posed by increasing population ageing.
Assistive technologies to enhance quality of life of older people
Background
While life expectancy (LE) is increasing globally, healthy life expectancy (HLE) is not increasing at the same pace. As such, in some settings, people are living longer with additional years of disability. This gap between LE and HLE is associated with progressive loss of physical, mental and cognitive integrity, overall affecting the activities of daily life (ADL) and quality of life of older people. Older people could be affected by a progressive loss of muscle mass and function, a condition referred to as “sarcopenia”, which is present in 1 to 50% of community-dwelling older adults. Physical inactivity contributes to the development of sarcopenia, and among older adults, this risk is accrued due to high burden of disease-related immobility or disability. Decreased muscle mass and function leads to diminished muscle strength and increased vulnerability to falls, subsequently resulting in fractures, disability and death.
Improvement in physical capacity leads to improvement in functional capacity. The maintenance and improvement of physical function for older people is critical in retaining ADL and quality of life. New technologies are rapidly emerging and are showing great potential for monitoring physical activities for older people. Data and information captured by these new assistive technologies could help design programmes to improve physical activity, prevent gait disorders and improve quality of life of older people.
Goal
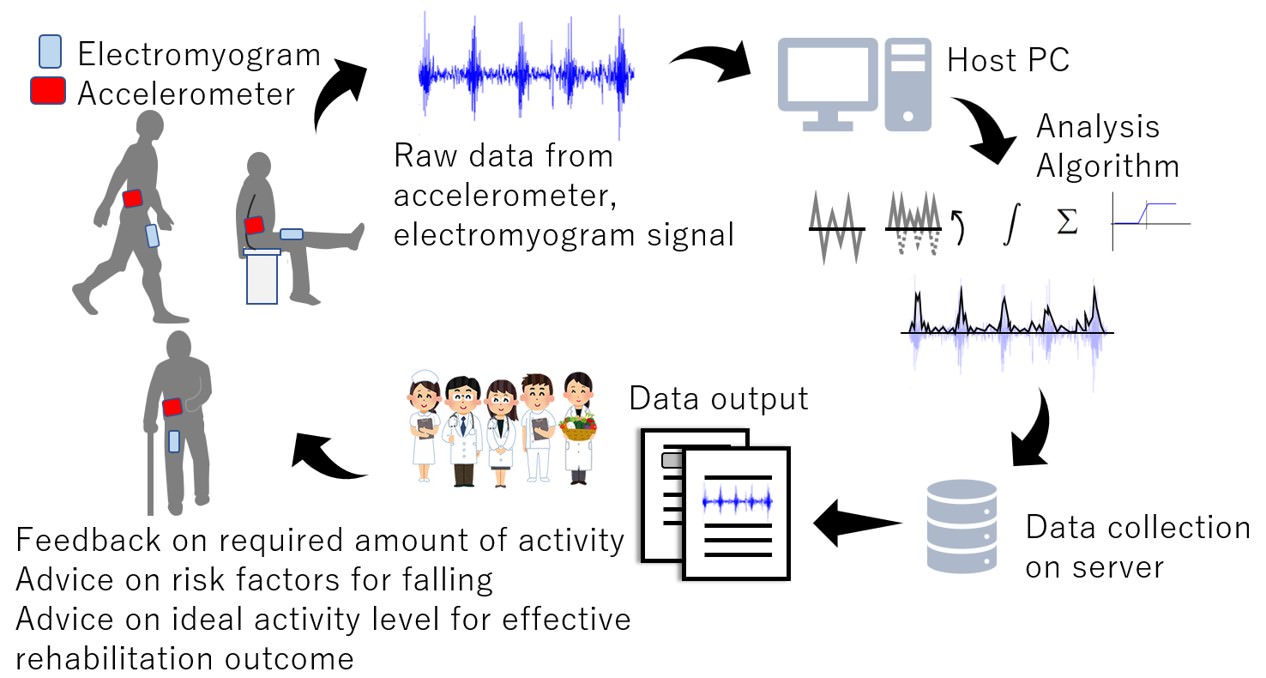
The goals of the research are three-fold:
- To develop a new algorithm for assessing the amount of physical activity required to maintain ADL and walking function among older adults.
- To document the patterns of falls and identify risks of specific physical activities and postures that affect the frequency of fall.
- To determine the optimum physical activity level for achieving better rehabilitation outcomes for inpatients.
Methods
This research consists of three parts. Part I is a pilot study involving 20 healthy volunteers (over 20 years) to measure physical activity through electromyogram (EMG) signals of the anterior thigh muscle. The new algorithm will be tested on a sample of 20 older adults aged 65 years and older. Part II is an observational study targeting 50 community-dwelling adults 65 years and older. Data about patterns of fall and physical activity were recorded using a non-invasive and validated accelerometer. Part III is an observational study of inpatients 20 years and older undergoing rehabilitation therapy for six types of conditions. Physical activity was measured using a validated accelerometer over seven continuous days from the start of the rehabilitation. In addition, body composition was measured using a portable medical body composition analyser.
Results
A significant positive correlation was found between the sum of root mean square of electromyographic signal and oxygen consumption during both ergometer exercise and walking. Preliminary data were collected among healthy subjects to develop a new application programme for the wearable accelerometer. Among inpatients, not increase in skeletal muscle mass was detected for hospitalized patients with chronic obstructive pulmonary disease (COPD) or heart failure who received conventional pulmonary or cardiac rehabilitation therapy.
Implications
The findings will contribute to an algorithm for estimating energy expenditure and to the development of a telemetry monitoring system for hospitalized patients. The lack of change in the mass of skeletal muscle in hospitalized patients, as shown in part III of the study, calls for a re-examination of the current pulmonary and cardiac rehabilitation programmes and exploration of new interventions.


Experiences of Assistive Products Use among Older People in Japan
Background
More than one billion of the world’s population need assistive technologies (AT). AT comprise a wide spectrum of products, ranging from ‘low-tech’ to ‘high-tech’ devices. Examples include, but are not limited to, hearing aids, glasses, walking frames, wheelchairs, communication aids, memory aids, and prostheses. Access to AT remains very limited with only one in ten people worldwide having access to such technology. Older people are one of the largest groups in need of assistive products and devices due to high prevalence of chronic morbidities and other age-related frailty and disabilities. There is limited research on the profile of people using AT, the types of AT that are used, as well as the users’ experience with AT among the oldest old. Japan, being the world’s leading aged society, offers a unique setting for addressing this research gap.
Goal
To document the profile of AT use, in terms of the age of the users, types of most commonly used AT, and the users’ experience with AT among the community-dwelling oldest old in Japan.
Methods
This is a cross-sectional, mixed-methods study. The quantitative arm consisted of a preliminary mail-based survey followed by a detailed face-to-face, interviewer-administered structured questionnaire. Participants were sampled from two specific studies: the Kashiwa90 study and the SONIC (Septuagenarians, Octogenarians, Nonagenarians Investigation with Centenarians) study. The Kashiwa90 study is a newly established cohort by this research project. It focuses on individuals 90 years and above residing in Kashiwa City. The SONIC is an ongoing prospective cohort study, initiated in June 2010, in the Kansai area (Itami City and Asago City of Hyogo prefecture) and Kanto area (Itabashi City and Nishitama district of Tokyo). The collected data consisted of the participants’ demographic characteristics, health status, physical condition, cognitive and motor functions, mental health, and other relevant information. The qualitative arm of the research consisted of in-depth interviews on users’ experience with AT.
Results
The analytical sample size for the mail survey included a total of 2,477 participants from both the Kashiwa90 and SONIC studies. The participants’ ages ranged from 88 to 106 years with 2.1% of them being aged 100 years and older. The majority (98.7%) used some type of AT. Multiple device use was very common. Around 79% of the participants reported using three or more AT, while the proportion of those who reported using at least five AT was 44.8%. The most commonly used AT included dentures (76.7%), glasses and other wearable vision-related devices (72.0%), handrails (51.4%), and canes (47.6%). Data from the qualitative interviews (one male and four females ranging in age from 94 to 100 years) revealed that the use of AT had a notable positive impact on daily living activities of the community-dwelling oldest old.
Implications
This study has shown the high prevalence of multiple AT use and has documented the most commonly used AT by community-dwelling oldest old in Japan. This information could inform the design and prescription of AT that are attuned to the needs of the oldest old. An important outcome of this research project is that it has set up a new research cohort, the Kashiwa90 study, which will potentially serve as a data source for future research on AT and other aging-related issues among the oldest old in Japan.


Health Metrics for Age-Friendly Environments
This project aimed to promote research and evaluation of Age-friendly Cities (AFC), and age-friendly environment initiatives more broadly. This, in turn, would lead to strengthening the evidence base for whole-of-society, multisectoral interventions to promote healthy ageing. The foundation for this work was the 2015 WKC publication, “Measuring Age-friendliness: A Guide to Using Core Indicators”. The main activities for the final year of this project were dissemination and awareness-raising through publications, presentations at international meetings and conferences, and capacity building.
For current information on WHO’s initiative on Age-friendly Environments, please visit: http://www.who.int/ageing/age-friendly-environments/en/

Health Technology Assessment: A prioritization exercise
Many new technologies are being developed to promote health among older adults. This report identifies prioritisation criteria for the selection of health technologies for older adults facing declining functional capacity, with the focus on low- and middle-income countries. The criteria were then evaluated on a horizon scanning system to identify promising health technologies for older adults.
Methods
A rapid review of major scientific databases, including MEDLINE, EMBASE™ and the Cochrane Library, were searched for relevant studies from January 1 2000 to September 1 2017, and supplemented with targeted searches using Google and Google Scholar. A review of existing horizon scanning systems was performed to examine prioritisation criteria and processes that have been used to prioritise emerging health technologies. The compiled criteria were applied to a publicly available compilation of health technologies developed by the Canadian Agency for Drugs and Technologies in Health (CADTH) in order to perform an identification exercise. The compilation contains 66 emerging health technologies identified in late-2016 and the first six months of 2017. All technologies identified by CADTH were reviewed in order to filter those relevant for the target population. As a result, 25 technologies were included in the prioritization exercise. Finally, these 25 technologies were examined against criteria designed for the population of older adults.
Findings
The prioritisation criteria were grouped into eight areas: need, clinical benefit, cost, evidence base, equity and equality, personal wellbeing, patient autonomy and culture. The identification exercise resulted in six health technologies that have the potential to improve health and quality of life of target population.
Discussion and conclusions
The criteria reflect the needs of the population of older adults who experience decline in their physical and intrinsic capacity, and present factors that have the potential to influence further acceptance and adoption of new technologies. The developed criteria can be applied on various information sources that collect data on emerging technologies, both in developed and developing countries. The findings of this report can be used to inform the future prioritisation process for the target population. Further research is necessary to define key public health problems of the population of older adults with the most urgent need for innovation in order to refine the existing criteria and formalise the prioritisation process.
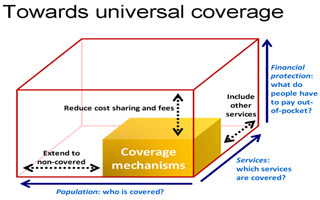
UHC Leadership Programme
Countries that have or will soon experience rapid population ageing have not fully understood the implications nor potential impact of the needs of population ageing on their health and social delivery systems. Planning for health systems strengthening towards UHC offers a major opportunity to transform systems and to appropriately plan for their future. Working across sectors and engaging communities are essential strategies, as is the need to ensure equity.
Given that countries are still at the early stage of addressing population ageing, this effort is a step to assist them develop trajectories (or roadmaps) for health system design, service delivery and financing in their contexts. The Leadership programme is helping to advance and accelerate their UHC agenda by supporting the country counterparts (as individuals and as country teams) with leadership training, coalition building support and results-oriented collective action initiatives. A key focus is to help define the “how to” for navigating and shaping the political economy in each country for the ageing and UHC agenda.
This UHC Leadership Programme is one of the opportunities to share evidence, data, information and case models for future policy options to the UHC leader in low and middle income countries. This programme is implemented in collaboration with Kanagawa Prefecture, Japan.
The objectives of the programs were to:
1. Share national/local decision making to lead, advocate, advance, design and implement reforms and programmes to transform health/social service delivery systems for ageing populations to attain UHC.
2. Share lessons and insights from Japan and among Asian countries for systems to respond to the needs of ageing population.
3. Share information and experience among countries to enable countries to develop initial trajectories (or roadmaps) for pursuing actions in their countries.
4. Provide lessons and examples from leading countries (e.g., Japan, Singapore) and from WHO synthesized knowledge for major components of health and social service systems design to support ageing populations: a) identifying a wide set of potential required services (coverage) b) models of delivery systems (and tailoring to each country needs); c) financing strategies d) health workforce implications e) use of technology and f) related enabling governance strategies.

Community-Based Social Innovations
Health systems across both developed and developing regions struggle to meet the diverse and complex needs of increasing number of older persons. We hypothesized that community based social innovations (CBSIs) can improve the health and well-being of older people through community-based care. This research therefore, endeavored to answer the following questions through case studies in 14 countries:
1) What are CBSIs?
2) Are CBSIs effective and cost-effectiveness in promoting healthy ageing?
3) What typology can help advance understanding of CBSIs at the operational level to enable
implementation?
Results
This research defined CBSIs as community initiatives that seek to: a) empower older people to improve their self-efficacy in caring for themselves and their peers; b) maintain their well-being and; c) promote social cohesion and inclusiveness.
When considering the range of ‘health’ impacts from the CBSIs, we employed the term ‘health’ very broadly – incorporating for example physical and mental health, as well as broader well-being. In terms of understanding CBSI’s effectiveness therefore, we found that:
- The main health benefits important for individuals and communities are often psycho-social, for example, the integration of socially isolated older people into mainstream community and society.
- CBSIs can lead to people-centred services through engagement and empowerment by, for example, increasing awareness and knowledge that helps older people and their families in navigating complex health and social care options. CBSIs also empower informal carers –many of whom are women.
Challenges to wider scale and equitable implementation exist for several reasons. Many CBSIs rely on volunteers or older people themselves as agents of change. Linkages to immediate health and social care systems are often limited. In addition, strategic planning remains a weakness as does the reliability and availability of long-term funding.
The great diversity of models and lack of robust monitoring and evaluation frameworks impeded evaluation of cost-effectiveness. The CBSIs studied varied widely in terms of aims, scope, setting, activities, governance and funding. Nevertheless, CBSIs could be categorised by level of empowerment, linkages to the health and social care system, and their scale, scope and complexity. Using these categories, we identified four ‘types’ of CBSI, each with strengths and challenges:
Way forward
In many cases, CBSIs begin as community initiatives that fill gaps in services that the community needs. However, such models may not be sustainable, because they are too dependent on voluntary commitment. Formal linkages with the health sector are essential, requiring a recognition of the needs of older people in national and regional policies. Future research will emphasize innovations in community-based service delivery, with an aim to assess generalizability, validity, replicability and scale-up potential.

Technology and social innovations for an ageing Asia
In March 2016, the WHO Kobe Centre was invited to participate in a workshop on Comparative Ageing Policies in Asia at the Lee Kuan Yew School of Public Policy, National University of Singapore. There, participants developed the outline for a book, entitled “Ageing in Asia”, to be published in 2018. This book will offer an overview of how ageing influences policies throughout Asia, and cover social, economic and demographic trends, health and social issues relevant to the health of older people, and the role of technology and social innovations.
Objectives
The WHO Kobe Centre prepared the chapter “Technological and social innovations for an ageing Asia”. The chapter comprised of (a) a review of social innovations that support the re-alignment of health and social policies in response to population ageing; and (b) a review of innovative technologies and the role of Health Technology Assessments in health and social care for ageing populations.
Results
The review of (a) focused on three policy domains: pension and financial security, universal health coverage, and community-based approaches.
Experiences in Japan and the Republic of Korea have demonstrated that improving pension systems have yielded significant benefits in providing safety nets for older people, including protection from catastrophic health expenditure. Other parts of Asia would benefit from innovations in pension schemes to provide financial security for demographics with limited pension entitlements. Policies relying on family caregiving also need to be addressed.
The adoption of universal health insurance in Japan in 1961 has contributed greatly toward the achievement of universal health coverage. Even in countries with universal health insurance, however, out-of-pocket expenditures and health care costs are problematic for older persons on a low or fixed budget. High out-of-pocket costs also increase inequities in access to health technologies. Countries such as China will have to address growing shortages of health workers. Social innovations will support universal health coverage in Asia by addressing gaps in health systems and policies.
Social innovations that supplement services offered by state institutions have had a largely positive impact throughout Asia. Successful community-based interventions in Viet Nam and Japan have empowered older people to retain their well-being even in the face of disease, disability, and health decline.
The review of (b) revealed low-cost, disease-specific products, such as smartphone applications in India to manage physical disabilities after a stroke, to more costly ones with broader application, such as exoskeletons used by older workers in Japan. Assistive health technologies that maintain function at older age is a particularly active area for innovation. Wider adoption of telemedicine and remote monitoring systems has the potential to make home-based care safer and accessible, especially in remote areas. Mobile health (mHealth) technology services can improve monitoring of chronic conditions and function in older people, as demonstrated in China with older diabetics and their family caregivers. Further research is needed, however, to ensure that mHealth technologies are appropriately designed and targeted to the end-users’ needs.
Health technology assessments (HTA) have been implemented in several countries to support decision-making processes and health reforms, especially with regards to facilitating market entry, providing insurance coverage, and ensuring accessibility of technologies for older adults. Asia has been a leader in developing HTA. Most HTA agencies in the region are now part of the HTA Asia Link Network as well as the International Network of Agencies for Health Technology Assessment (INAHTA). To realize the full potential of technological innovations, strategic partnerships between industry, NGOs, and governments are needed for policies and regulations that create accessible, affordable, and appropriate innovations that deliver impact at scale.