National Reporting Instrument 2021
Background
[iBG]
Adopted in 2010 at the 63rd World Health Assembly (WHA Res 63.16), the WHO Global Code of Practice on the International Recruitment of Health Personnel (“the Code”) seeks to strengthen the understanding and ethical management of international health personnel recruitment through improved data, information, and international cooperation.
Article 7 of the Code encourages WHO Member States to exchange information on the international recruitment and migration of health personnel. The WHO Director General is additionally mandated to report to the World Health Assembly every 3 years.
WHO Member States completed the 3rd round of national reporting in March 2019. The WHO Director General reported progress on implementation to the 72nd World Health Assembly in May 2019 (A 72/23). The 3rd Round of National Reporting additionally informed the Member-State led Review of the Code’s relevance and effectiveness, as presented to the 73rd WHA in 2020 (A 73/9).
The Review highlights that Code implementation, through targeted support and safeguards, is necessary to ensure that Health Emergency and Universal Health Coverage-related progress in Member States serves to reinforce rather than compromise similar achievement in others. In light of the considerations in the Report and decision WHA 73(30), the WHO Secretariat has additionally prepared the Health Workforce Support and Safeguards List, 2020.
The National Reporting Instrument (NRI) is a country-based, self-assessment tool for information exchange and Code monitoring. The NRI enables WHO to collect and share current evidence and information on the international recruitment and migration of health personnel. The findings from the 4th Round of National Reporting are to be presented at the 75th World Health Assembly in May 2022. Given the ongoing COVID-19 pandemic, the NRI (2021) has been adapted to additionally capture information related to health personnel recruitment and migration in the context of the pandemic.
The deadline for submitting reports is 31 January 2022.
Should technical difficulties prevent national authorities from filling in the online questionnaire, it is also possible to download the NRI via the link: https://www.who.int/teams/health-workforce/migration/code-nri. Please complete the NRI and submit it, electronically or in hard copy, to the following address:
Health Workforce Department
Universal Health Coverage and Health Systems
World Health Organization
20 Avenue Appia, 1211 Geneva 27
Switzerland
hrhinfo@who.int
Disclaimer: The data and information collected through the National Reporting Instrument will be made publicly available via the WHO web-site following the proceedings of the 75th WHA in 2022. The quantitative data collected will be updated on and available through the National Health Workforce Accounts online platform. (http://www.who.int/hrh/statistics/nhwa/en/).
Article 7 of the Code encourages WHO Member States to exchange information on the international recruitment and migration of health personnel. The WHO Director General is additionally mandated to report to the World Health Assembly every 3 years.
WHO Member States completed the 3rd round of national reporting in March 2019. The WHO Director General reported progress on implementation to the 72nd World Health Assembly in May 2019 (A 72/23). The 3rd Round of National Reporting additionally informed the Member-State led Review of the Code’s relevance and effectiveness, as presented to the 73rd WHA in 2020 (A 73/9).
The Review highlights that Code implementation, through targeted support and safeguards, is necessary to ensure that Health Emergency and Universal Health Coverage-related progress in Member States serves to reinforce rather than compromise similar achievement in others. In light of the considerations in the Report and decision WHA 73(30), the WHO Secretariat has additionally prepared the Health Workforce Support and Safeguards List, 2020.
The National Reporting Instrument (NRI) is a country-based, self-assessment tool for information exchange and Code monitoring. The NRI enables WHO to collect and share current evidence and information on the international recruitment and migration of health personnel. The findings from the 4th Round of National Reporting are to be presented at the 75th World Health Assembly in May 2022. Given the ongoing COVID-19 pandemic, the NRI (2021) has been adapted to additionally capture information related to health personnel recruitment and migration in the context of the pandemic.
The deadline for submitting reports is 31 January 2022.
Should technical difficulties prevent national authorities from filling in the online questionnaire, it is also possible to download the NRI via the link: https://www.who.int/teams/health-workforce/migration/code-nri. Please complete the NRI and submit it, electronically or in hard copy, to the following address:
Health Workforce Department
Universal Health Coverage and Health Systems
World Health Organization
20 Avenue Appia, 1211 Geneva 27
Switzerland
hrhinfo@who.int
Disclaimer: The data and information collected through the National Reporting Instrument will be made publicly available via the WHO web-site following the proceedings of the 75th WHA in 2022. The quantitative data collected will be updated on and available through the National Health Workforce Accounts online platform. (http://www.who.int/hrh/statistics/nhwa/en/).
[hidLabels]
//hidden: Please not delete.
Please describe
Disclaimer
[disclaim]
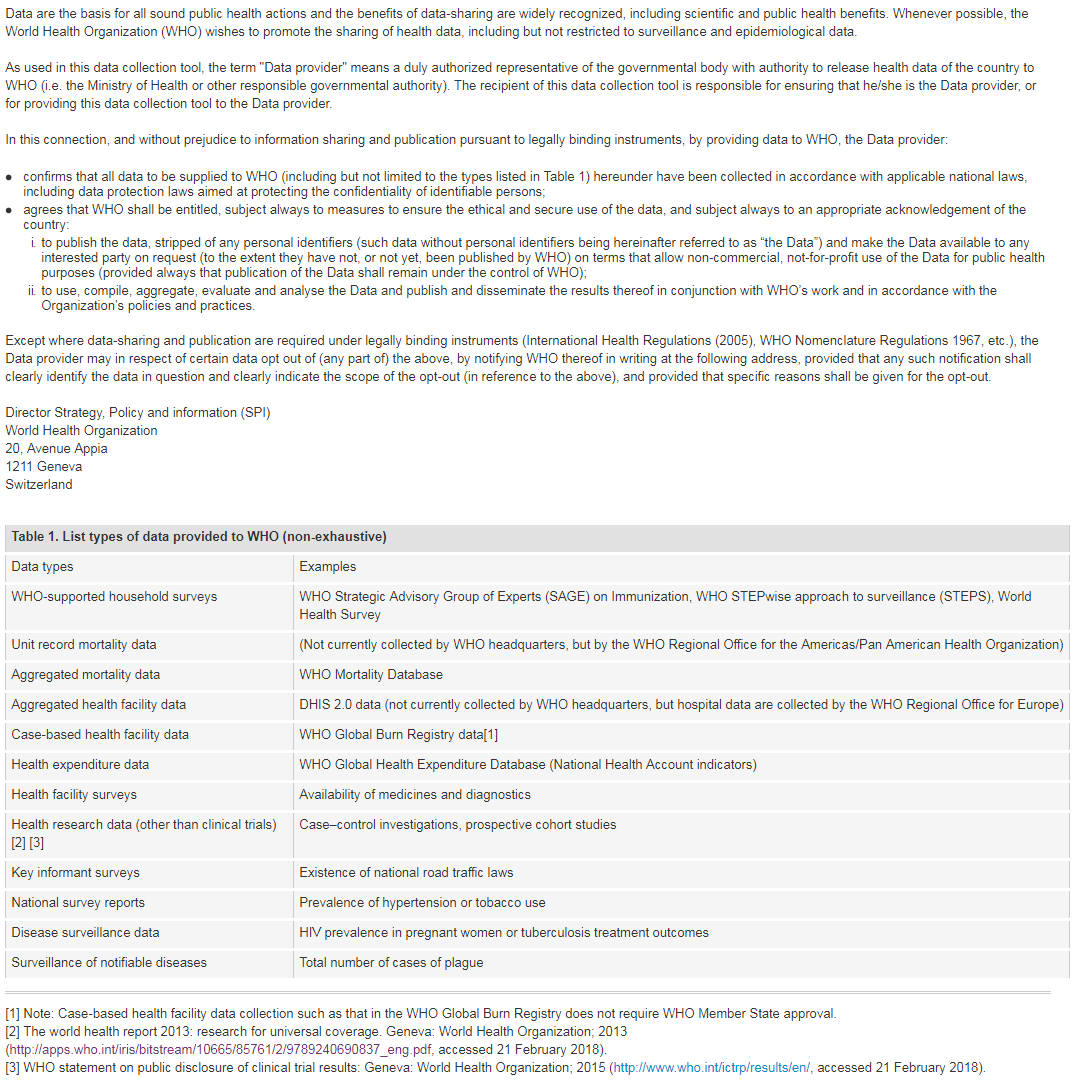
For more information on WHO Data Policy kindly refer to http://www.who.int/publishing/datapolicy/en/
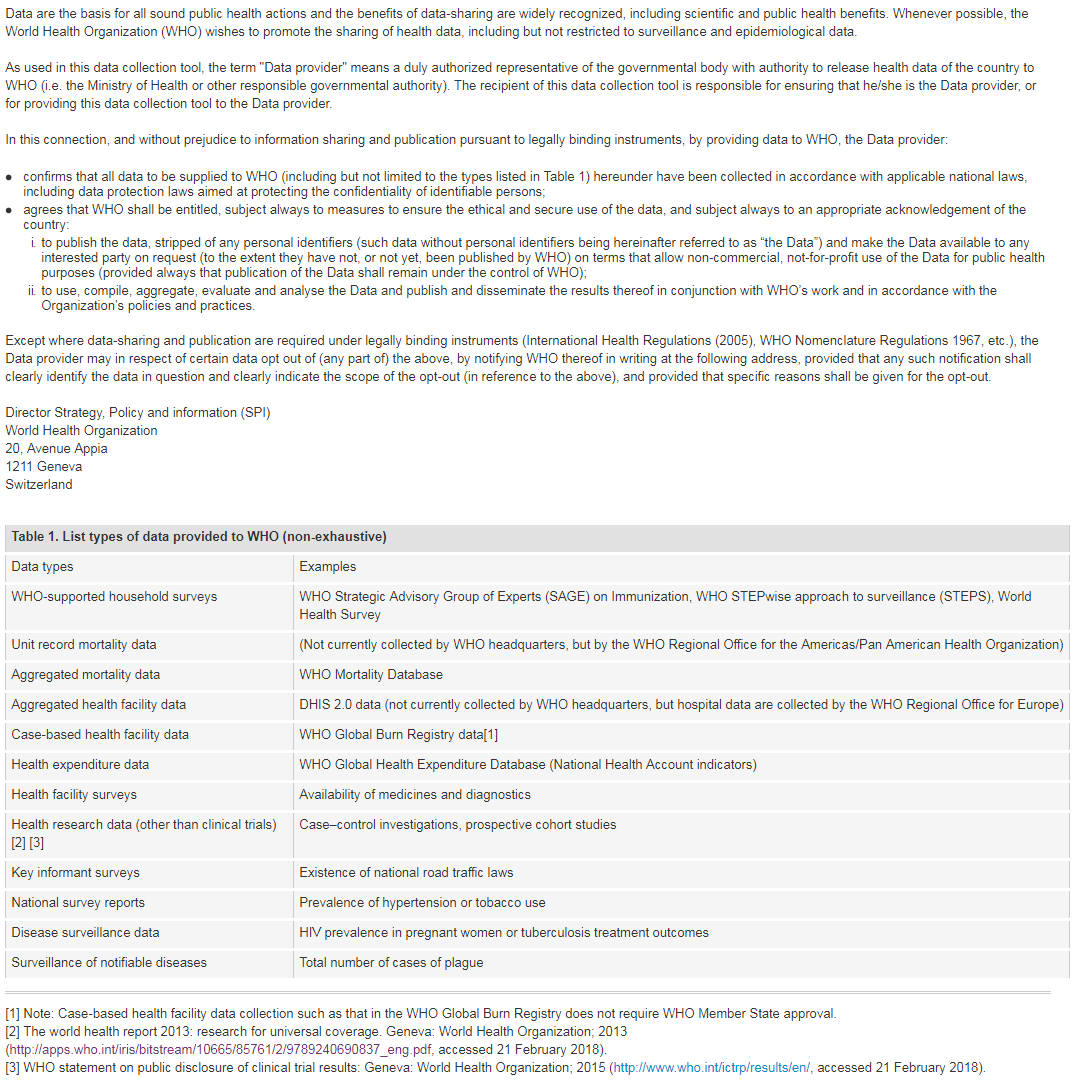
For more information on WHO Data Policy kindly refer to http://www.who.int/publishing/datapolicy/en/
I have read and understood the WHO policy on the use and sharing of data collected by WHO in Member States outside the context of public health emergencies
Designated National Authority Contact Details
[q01b]
Contact information:
Country
United Kingdom of Great Britain and Northern Ireland
Full name of institution:
Sarah
Name of designated national authority:
Sarah Cliff
Title of designated national authority:
Mrs
Telephone number: (E.g. +41227911530 .)
01132546275
Email: (Please enter one email address only.)
sarah.cliff@dhsc.gov.uk,hrhinfo@who.int
Implementation of the Code
[q1]
1. Has your country taken steps to implement the Code?
Yes
[q1x1x]
1.1 Actions have been taken to communicate and share information across sectors on the international recruitment and migration of health personnel, as well as to publicize the Code, among relevant ministries, departments and agencies, nationally and/or sub-nationally.
Yes
[q1x1]
Action 1
In February 2021, the Department of Health and Social Care published a revised Code of Practice for the International recruitment of health and social care personnel. This builds on the Code of Practice first published in 2004 and implements the WHO Global Code of Practice in a UK setting. It takes account of the WHO Expert Advisory Group recommendations in the report WHO A73/9.
The updated Code has been widely publicised via the GOV.UK website, NHS Employers website, media, social media, webinars and presentations at stakeholder meetings across the health and social care sectors including:
- Cross Government groups
- Trade Unions
- Agencies
- Professional Regulatory Bodies
- Health and social care professional bodies
- NHS organisations
- NHS international recruitment leads network meetings
- Independent sector network
- International nursing associations
The Code of Practice has also reached international audiences and was show cased at the following webinars/events:
- German Network/Hospeem webinar (followed by publication of an article on fair recruitment in German magazine IQ konkret)
- THET sustainable workforce symposium
- WHO tri-regional meeting on the International Mobility of Health Professionals
Devolved Administrations
The revised Code of Practice policy is UK wide. Each devolved nation adheres to the aims, objectives, guiding principles and best practice benchmarks of the Code of Practice, but holds its own Code of Practice to reflect the different organisational structures in each nation.
Scotland has published a Scottish Code of Practice for the International Recruitment of Health and Social Care Personnel.
Wales and Northern Ireland are planning to publish their own versions of the Code in September 2021 subject to Ministerial approval.
NHS Wales organisations are also committed to the provisions of the Welsh Government’s Code of Practice: ethical employment in supply chains. The code commits public, private and third sector organisation in Wales to a set of actions to tackle illegal and unfair employment practices.
Action 2
NHS Employers has a lead role in implementing the UK Code of Practice by managing and hosting the list of agencies that adhere to the Code of Practice.
NHS Employers hosts information about the Code of Practice and the agency list on its website and undertakes communications activity to promote the Code of Practice. It also provides a dedicated advice and support service to health and care organisations to help them to follow the guiding principles of the Code of Practice in all their recruitment activities.
The NHS Employers’ international recruitment toolkit has been designed to support collaborative, effective and ethical international recruitment and encourage and enable supportive practices and processes for the recruitment of international staff across a wide range of professions. NHS Employers also has developed a range of promotional material to support the Code of Practice including a quick guide to the Code of Practice, frequently asked questions, video presentation, and top tips for working with agencies.
NHS Employers also provide a mechanism for stakeholders across the system to promote the Code of Practice, assess activity and, if necessary, challenge poor practice with employers and agencies.
Action 3
[q1x2x]
1.2 Measures have been taken or are being considered to introduce changes to laws or policies consistent with the recommendations of the Code.
Yes
[q1x2]
Measure 1
The UK Code of Practice has been updated to reflect the present situation and to align with the WHO Expert Advisory Group recommendations in the report WHO A73/9.
Updates include:
• Preventing active recruitment from 47 countries on the WHO Health Workforce Support and Safeguards List, 2020, unless there is a Government to government agreement, and the inclusion of a definition of “active recruitment” to ensure clarity for recruiting organisations;
• A refresh of the list of recruitment agencies signed up to operating in accordance with the code to reaffirm their commitment to the new Code if they wish to continue to recruit internationally;
• Strengthening guidance to ensure international recruits will be treated fairly, receive the same terms and conditions as UK workers and be provided with the appropriate support;
• Setting out how the UK is supporting countries with the most pressing health and social care workforce challenges.
• Broadening the scope to include the social care sector and the UK’s Devolved Administrations (Scotland, Wales and Northern Ireland);
• An increased focus on monitoring of recruitment activity, in particular on workforce flows from middle income countries and fragile and conflict-affected states.
Measure 2
NHS England and Improvement (NHS EI) provide financial support to NHS Trusts for nursing international recruitment. This will be extended to midwifery international recruitment in 2021/22.
An important condition in the Memorandum of Understanding between NHSEI and NHS Trusts on them accessing this funding, is that all their international recruitment activity must adhere to the Code of Practice. In particular, ensuring NHS Trusts do not actively recruit health and care professionals from a country on the WHO Health Workforce Support and Safeguards list unless there is a government-to-government agreement in place. NHS EI monitor nurse joiner information and will engage with NHS trusts if there appears to be a flow from countries on the WHO list. This will be a key responsibility of the regional International Recruitment lead to maintain going forward.
Measure 3
NHS Employers routinely check agency compliance with the code through spot checks and biennial reviews, responds to complaints or other information with regard to potential breaches, and takes necessary action as set out in Annex C of the Code; process for code of practice contraveners. More information on the process is set out at 1.3.
NHE EI also encourages NHS Trusts, when recruiting internationally to ensure the agency they use is recruiting ethically, and to escalate any concerns to NHS Employers or via NHS EI. Trusts are advised that they should be considering the following types of questions to ensure ethical recruitment:
• Whether an agency is signed up to the code of practice and follow the guiding principles and best practice benchmarks, for example not charging a fee to the recruit;
• Where an agency actively recruits from;
• If an application is received from a health or care professional from a country on the WHO Health Workforce Support and Safeguards list, probing questions should be asked to understand whether or not an agency played a part in them becoming aware of a post or applying.
[q1x3x]
1.3 Records are maintained on all recruiters authorized by competent authorities to operate within their jurisdiction.
Yes
[q1x3]
Please describe:
NHS Employers has a lead role in implementing the UK Code of Practice by managing and hosting the list of agencies that adhere to the Code of Practice. Health and care organisations should only use agencies which appear on this list. Applications Recruitment agencies wishing to apply to be placed on the Code of Practice list of agencies for international recruitment are required to complete an application form. The application form confirms: • the agency's commitment to fully adhere to the Code of Practice; • the business practice of the agency; • a declaration of all associated business activities relating to the commercial recruitment of healthcare professionals. If, after examination of the application and resolution of any queries, an agency is not successful in being placed on the list, they will be advised of the reason in writing via email. The agency must wait three months before it can re-apply and must show that it has changed its business practice in order to be successfully placed on the list. Audits and spot checks An audit (biennial review) of agency details held on the list is undertaken every two years and agencies are required to provide evidence that they are still in full compliance with the CoP by self-certification, complete a new application and reaffirm their commitment to the Code, review agency website and social media, as well as provide up to date contact details. Reporting NHS Employers report to the Department of Health and Social Care on a monthly basis identifying total numbers of agencies on the list, including investigation details and any additions and removals from lists explaining why this is the case. Accurate and up to date records of all agencies are maintained through a secure NHS Employers system as well as an accessible version on NHS Employers website. Agency List Refresh When an updated version of the Code of Practice was published in February 2021, NHS Employers undertook a refresh of the list of recruitment agencies to reaffirm their commitment to the new Code if they wish to continue to recruit internationally. The refresh has reduced the number of agencies from 688 to 320. The reduction is largely owing to many agencies historically being on the list even though they did not undertake international recruitment or because they are no longer trading. The smaller number of agencies on the list will allow tighter monitoring going forward.
[q1x4x]
1.4 Good practices, as called for by the Code, are encouraged and promoted among recruitment agencies.
Yes
[q1x4]
Please describe:
1.4.1 Promotion of the Code among private recruitment agencies.
NHS Employers encourages and promotes good practices among recruitment agencies and as referred to in 1.3, manages and hosts the list of agencies that adhere to the Code of Practice as well as developing web pages and other promotional material about the Code. Health and Social Care employers must only use agencies on the agency list. The Agency List refresh, undertaken when the updated Code was published, ensured every agency on the list is aware of, and is signed up to the new Code of Practice. NHS Employers also has a continuous relationship with NHSEI approved international framework operators to share best practice and knowledge of implementation of the Code of Practice. DHSC has set up quarterly meetings with recruitment agencies to promote the code, share best practice and ensure agencies are kept up to date on the policy direction in the international recruitment space. These meetings are open to any recruitment agency who wish to attend.
1.4.2 Domestic legislation or policy requiring ethical practice of private recruitment agencies, as consistent with the principles and articles of the Code.
This is described in 1.3.
1.4.3 Public or private certification of ethical practice for private recruitment agencies.
This is described in 1.3
1.4.4 Others
[q1x5x]
1.5 Measures have been taken to consult stakeholders in decision-making processes and/or involve them in activities related to the international recruitment of health personnel.
Yes
[q1x5]
Measure 1
The UK Government has increased its oversight of international recruitment in recent years, including the impact on source countries, through the formation of a Cross-Whitehall International Recruitment Steering Group for Health. The Steering Group brings together key Government Departments, the devolved administrations and key system partners to provide national policy oversight and collaboration on international recruitment workforce supply.
The Steering Group oversaw the review of the Code of Practice, and approved all changes and updates made to the Code. It will undertake a further review of the Code, one year after publication.
A wide range of other stakeholders were involved in the review and had the opportunity to comment and shape the revised code. These included, the WHO, Health Trade Unions, Professional Bodies, Professional Regulatory organisations, healthcare employers and social care representative organisations.
Measure 2
NHS Employers routinely engages with employers about their international recruitment activity through their networks, forums, groups and surveys. In instances when they are asked or made aware about potential recruitment opportunities from a country included on the WHO Health Workforce Support and Safeguards list, 2020, they reiterate the up to date information provided on their website. They also have regular dialogue with key stakeholders to ensure they are aware of related activities and information.
Measure 3
[q1x6x]
1.6 Other steps:
No
Partnerships, Technical Collaboration and Financial Support 1/2
[q2x1]
2.1. Has your country provided technical or financial assistance to one or more WHO Member States, particularly developing countries, or other stakeholders to support the implementation of the Code?
2.1.1 Specific support for implementation of the Code
2.1.2 Support for health system strengthening
2.1.3 Support for health personnel development
2.1.4 No support provided
2.1.5 Other areas of support:
[q2x2]
2.2. Has your country received technical or financial assistance from one or more WHO Member States, the WHO secretariat, or other stakeholders to support the implementation of the Code?
2.2.1 Specific support for implementation of the Code
2.2.2 Support for health system strengthening
2.2.3 Support for health personnel development
2.2.4 No support received
2.2.5 Other areas of support:
Partnerships, Technical Collaboration and Financial Support 2/2
[q3]
3. Has your country or its sub-national governments entered into bilateral, multilateral, or regional agreements and/or arrangements with respect to the international recruitment and migration of health personnel?
Yes
[q3xTitle]
Title of Agreement
| Title | Web-link to agreement | Upload the full text of the agreement | |
|---|---|---|---|
| Agreement 1 | Bilateral Agreement Between the Government of the Republic of Kenya and the Government of the United Kingdom and Northern Ireland for collaboration Health Care Workforce | TBC | |
| Agreement 2 | Memorandum of Understanding Between the Government of the Republic of the Philippines and the Government of the United Kingdom of Great Britain and Northern Ireland on Healthcare Cooperation | ||
| Agreement 3 | Memorandum of Understanding for International Cooperation on Health Professional Development | ||
| Agreement 4 | MoU for a partnership on nursing between HEE and Saint Vincent and the Grenadines | ||
| Agreement 5 |
[q3xUploadx1]
[q3xUploadx2]
[q3xUploadx3]
No comment
[q3xUploadx4]
[q3xUploadx5]
[q3xTOA]
If you cannot share the full text of the agreement please fill :
| Type of Agreement | Coverage | |
|---|---|---|
| Bilateral Agreement Between the Government of the Republic of Kenya and the Government of the United Kingdom and Northern Ireland for collaboration Health Care Workforce (SQ001) | Bilateral (A1) | National (A1) |
| Memorandum of Understanding Between the Government of the Republic of the Philippines and the Government of the United Kingdom of Great Britain and Northern Ireland on Healthcare Cooperation (SQ002) | Bilateral (A1) | National (A1) |
| Memorandum of Understanding for International Cooperation on Health Professional Development (SQ003) | Bilateral (A1) | National (A1) |
| MoU for a partnership on nursing between HEE and Saint Vincent and the Grenadines (SQ004) | Bilateral (A1) | National (A1) |
| (SQ005) |
[q3xMCA]
Main content of agreement
(check all that apply)
| Education and training | Institutional capacity building | Promotion of circular migration | Retention strategies | Recognition of health personnel | Recruitment of health personnel | Twinning of health care facilities | Other mechanism (include details if possible): | |
|---|---|---|---|---|---|---|---|---|
| Bilateral Agreement Between the Government of the Republic of Kenya and the Government of the United Kingdom and Northern Ireland for collaboration Health Care Workforce | 1 | 1 | 1 | |||||
| Memorandum of Understanding Between the Government of the Republic of the Philippines and the Government of the United Kingdom of Great Britain and Northern Ireland on Healthcare Cooperation | 1 | 1 | ||||||
| Memorandum of Understanding for International Cooperation on Health Professional Development | 1 | |||||||
| MoU for a partnership on nursing between HEE and Saint Vincent and the Grenadines | 1 | 1 | 1 | 1 | ||||
[q3xCHP]
Categories of Health Personnel (check all that apply)
| Doctors | Nurses | Midwives | Dentists | Pharmacists | Other (include details as necessary) : | |
|---|---|---|---|---|---|---|
| Bilateral Agreement Between the Government of the Republic of Kenya and the Government of the United Kingdom and Northern Ireland for collaboration Health Care Workforce | 1 | |||||
| Memorandum of Understanding Between the Government of the Republic of the Philippines and the Government of the United Kingdom of Great Britain and Northern Ireland on Healthcare Cooperation | 1 | |||||
| Memorandum of Understanding for International Cooperation on Health Professional Development | 1 | |||||
| MoU for a partnership on nursing between HEE and Saint Vincent and the Grenadines | 1 | |||||
[q3xVP]
Validity period
| From: | To: | |
|---|---|---|
| Bilateral Agreement Between the Government of the Republic of Kenya and the Government of the United Kingdom and Northern Ireland for collaboration Health Care Workforce (SQ001) | 2021 (2021) | 2024 (A27) |
| Memorandum of Understanding Between the Government of the Republic of the Philippines and the Government of the United Kingdom of Great Britain and Northern Ireland on Healthcare Cooperation (SQ002) | 2021 (2021) | 2024 (A27) |
| Memorandum of Understanding for International Cooperation on Health Professional Development (SQ003) | 2020 (2020) | 2023 (A28) |
| MoU for a partnership on nursing between HEE and Saint Vincent and the Grenadines (SQ004) | 2019 (2019) | 2023 (A28) |
| (SQ005) |
[q3xCN]
Countries that are involved
Bilateral Agreement Between the Government of the Republic of Kenya and the Government of the United Kingdom and Northern Ireland for collaboration Health Care Workforce
Kenya and the UK
Memorandum of Understanding Between the Government of the Republic of the Philippines and the Government of the United Kingdom of Great Britain and Northern Ireland on Healthcare Cooperation
Philippines and the UK
Memorandum of Understanding for International Cooperation on Health Professional Development
Thailand and the UK
MoU for a partnership on nursing between HEE and Saint Vincent and the Grenadines
Saint Vincent and the Grenadines and the UK
[q3xSYC]
Signatory of the agreement from your country
| Ministry of Foreign Affairs | Ministry of Health | Ministry of Education | Ministry of Trade | Ministry of Labour | Ministry of Immigration /Home Affairs | Other: | |
|---|---|---|---|---|---|---|---|
| Bilateral Agreement Between the Government of the Republic of Kenya and the Government of the United Kingdom and Northern Ireland for collaboration Health Care Workforce | 1 | ||||||
| Memorandum of Understanding Between the Government of the Republic of the Philippines and the Government of the United Kingdom of Great Britain and Northern Ireland on Healthcare Cooperation | 1 | ||||||
| Memorandum of Understanding for International Cooperation on Health Professional Development | 1 | ||||||
| MoU for a partnership on nursing between HEE and Saint Vincent and the Grenadines | 1 | ||||||
[q3xSYCOth]
Signatory of the agreement from your country (Please specify:)
Bilateral Agreement Between the Government of the Republic of Kenya and the Government of the United Kingdom and Northern Ireland for collaboration Health Care Workforce
Memorandum of Understanding Between the Government of the Republic of the Philippines and the Government of the United Kingdom of Great Britain and Northern Ireland on Healthcare Cooperation
Memorandum of Understanding for International Cooperation on Health Professional Development
Interim Chief Executive of Health Education England
MoU for a partnership on nursing between HEE and Saint Vincent and the Grenadines
Interim Chief Executive of Health Education England
[q3xSPC]
Signatory of the agreement from the partner country (ies)
| Ministry of Foreign Affairs | Ministry of Health | Ministry of Education | Ministry of Trade | Ministry of Labour | Ministry of Immigration /Home Affairs | Other: | |
|---|---|---|---|---|---|---|---|
| Bilateral Agreement Between the Government of the Republic of Kenya and the Government of the United Kingdom and Northern Ireland for collaboration Health Care Workforce | 1 | ||||||
| Memorandum of Understanding Between the Government of the Republic of the Philippines and the Government of the United Kingdom of Great Britain and Northern Ireland on Healthcare Cooperation | 1 | ||||||
| Memorandum of Understanding for International Cooperation on Health Professional Development | 1 | ||||||
| MoU for a partnership on nursing between HEE and Saint Vincent and the Grenadines | 1 | ||||||
[q3xSPCOth]
Signatory of the agreement from the partner country (ies) (Please specify:)
Bilateral Agreement Between the Government of the Republic of Kenya and the Government of the United Kingdom and Northern Ireland for collaboration Health Care Workforce
Memorandum of Understanding Between the Government of the Republic of the Philippines and the Government of the United Kingdom of Great Britain and Northern Ireland on Healthcare Cooperation
Memorandum of Understanding for International Cooperation on Health Professional Development
Secretary General Consortium of Thai Medical Schools
MoU for a partnership on nursing between HEE and Saint Vincent and the Grenadines
[q3xCOP]
Does the agreement explicitly reference the Code?
Bilateral Agreement Between the Government of the Republic of Kenya and the Government of the United Kingdom and Northern Ireland for collaboration Health Care Workforce
Yes
Memorandum of Understanding Between the Government of the Republic of the Philippines and the Government of the United Kingdom of Great Britain and Northern Ireland on Healthcare Cooperation
Yes
Memorandum of Understanding for International Cooperation on Health Professional Development
No
MoU for a partnership on nursing between HEE and Saint Vincent and the Grenadines
No
[q3xPAP]
Does the agreement reflect the code’s principles and practices?
Bilateral Agreement Between the Government of the Republic of Kenya and the Government of the United Kingdom and Northern Ireland for collaboration Health Care Workforce
Memorandum of Understanding Between the Government of the Republic of the Philippines and the Government of the United Kingdom of Great Britain and Northern Ireland on Healthcare Cooperation
Memorandum of Understanding for International Cooperation on Health Professional Development
Yes
MoU for a partnership on nursing between HEE and Saint Vincent and the Grenadines
Yes
Health Workforce Development and Health System Sustainability
[q4]
4. Does your country strive to meet its health personnel needs with its domestically trained health personnel, including measures to educate, retain and sustain a health workforce that is appropriate for the specific conditions of your country, including areas of greatest need?
Yes
[q4x1x]
4.1 Measures taken to educate the health workforce
Yes
[q4x1]
4.1.1 Manage production
4.1.2 Improve quality of education
4.1.3 Strengthen regulation
4.4 Others
[q4x2x]
4.2 Measures taken to ensure the sustainability* of the health workforce
Yes
[q4x2]
4.2.1 Workforce planning/forecasting
4.2.2 Increasing domestic production and education opportunities
4.2.3 Increasing employment opportunities
4.2.4 Manage recruitment of international health personnel
Other
[q4x3x]
4.3 Measures taken to address the geographical mal-distribution and retention of health workers*
Yes
[q4x3]
4.3.1 Education (Education institutions in underserved areas; students from under-served areas; relevant topics in education/professional development programmes; others)
England Measures to address geographical mal-distribution NHS England and NHS Improvement is funding a £20,000 salary supplement to attract GP trainees to work in areas of the country where GP training places have been unfilled for a number of years. Since its launch in 2016, the scheme has been successful in attracting GP trainees to areas of the country that have traditionally been hard to recruit to. Due to this success, NHS England and Improvement have provided additional funding to expand the number of places now available on the scheme to 500 from 2021. As part of the expansion of medical school places by 1,500 over recent years, five new medical schools have opened in historically hard-to-recruit areas, including rural and coastal locations across England. The bidding process for allocating the new places and schools prioritised areas with a relative shortage of doctors overall, and on the basis of schools’ commitment to social mobility and widening participation in medicine. Foundation Priority Programmes have also been introduced, beginning in 2019/20.This initiative, designed to attract and retain trainees in remote, rural and coastal geographies and shortage specialties, allows applicants to rank their preference for selected priority programmes as part of their application form. Successful applicants will be offered places on specific programmes prior to national allocation. Workforce Retention The NHS People Plan sets out a range of actions to transform people’s day to day experience of working in the NHS, focusing on the things that matter to staff including support for their wellbeing, improving flexible working opportunities and building a supportive and inclusive workplace culture. This will be an important step forward in helping the NHS to retain more staff. The Agenda for Change contract includes pay flexibilities to help attract and keep the staff the NHS needs. For example, in addition to basic pay, staff may receive High Cost Area Supplement payments if they work in and around London or local recruitment and retention premia if there are challenges in recruiting or retaining a particular job role. Scotland The Scottish Targeted Enhanced Recruitment Scheme offers a one off Grant of £20,000 (gross) to GP trainees committed to working in one of the identified training posts in Scotland that are in areas and programmes that have in the past proven difficult to recruit to. These areas often have an extremely good track record for education, but are initially less popular simply because of their geographical location. Trainees commit to an agreement to complete the three year training programme. If they leave the programme early, they will be required to pay back part of the funding. ScotGEM is a four-year graduate entry medical programme which commenced in 2018 and is designed to develop doctors who are interested in a career in general practice within NHS Scotland. The programme is tailored to meet the current and future needs of the NHS in Scotland and focuses on rural medicine and healthcare improvement. The programme is taught through a partnership between the universities of St Andrews and Dundee in collaboration with NHS Fife, NHS Tayside, NHS Highland, NHS Dumfries and Galloway and the University of the Highlands and Islands. Wales Since 2017 Welsh Government has funded a financial incentives of £20,000 to attract GP trainees to areas of Wales with a history of lower than average fill rates. The incentive is targeted at selected training areas within Hywel Dda University Health Board, Betsi Cadwaladr University Health Board (and Powys Teaching Health Board (‘PtHB’).
4.3.2 Regulation (Mandatory service agreements; scholarships and education subsidies with return of service agreements; enhanced scope of practice; task shifting; skill-mix; others)
Scotland Any student undertaking the ScotGEM programme is eligible to apply for a bursary of £4000 per year; totalling a maximum of £16,000 over the four year term. This is a return of service bursary meaning that for every year that the bursary is accepted, the student is expected to remain and work in NHS Scotland for one year following graduation i.e. if the bursary is accepted in all 4 years, the student will be bonded to working in NHS Scotland for 4 years post-graduation
4.3.3 Incentives (Financial and non-financial)
England Financial In July 2021 the Government announced that it was accepting the independent NHS Pay Review Body and Review Body for Doctors’ and Dentists’ Remuneration’s recommendations in full. This means that once implemented, all NHS staff within the two Review Bodies’ respective remit groups for this year, will receive a pay uplift of 3%, backdated to April 2021. The Review Bodies reached their 3% recommendation, taking into account the need to recruit, retain and motivate NHS staff. Some medical workforces, such as Doctors and Dentists in Training (Juniors) and some Specialty and Associate Specialist Doctors (SAS) are within respective multi-year pay and contract reform deals and therefore the Government did not ask the independent Review Body for Doctors’ and Dentists’ remuneration for a pay recommendation for these groups. For junior doctors, in 2019 the British Medical Association agreed to a multi-year pay and contract deal (2019/20-2022/23). The deal guarantees Junior Doctors pay scales will rise by a minimum of 8.2% over the four-year deal and includes an additional pay investment of circa £90 million. The deal also increases allowances for those working the most frequently at weekends, enhances eligibility for night shift pay, and creates a £1,000 a year allowance for Junior Doctors working less than full time, to assist with the cost of training. The multi-year pay and contract reform agreement for SAS doctors (reached in joint negotiations with the BMA) was introduced in April 2021. The agreement is a three-year deal covering the years 2021/22, 2022/23 and 2023/24. The deal offers SAS doctors faster progression to the top of the pay scales with meaningful increases at each progression point. The introduction of a new Specialist grade improves opportunities for career progression. The deal invested 3% per year. The range of benefits available to NHS staff exceeds that which is available in many other sectors, and the value of the total reward package has been increasing in recent years. Total reward is not just about pay and includes access to the NHS Pension Scheme, which is one of the best available, alongside a generous annual leave allowance and many additional benefits, such as support for learning and development. Non-financial Agenda for Change staff continue to see the benefits resulting from the previous multi-year pay and contract reform deal (2018/19-2020/21) which introduced many contractual changes such as putting learning and development at the centre of annual appraisal processes. The Government has introduced the Blended Learning nursing programme (BLP) which aims to address national shortages in clinical expertise by offering predominantly online remote-access study to those people who may have the aptitude and values to join the nursing profession, but currently are unable to learn in traditional ways. The Secretary of State confirmed the roll out of the BLP on the 8th July 2020 and HEE anticipate that around 8500 nurses will start training in BLPs over the next 5 years. The BLP programme is also being extended to midwifery degree programmes to start by September 2022.
4.3.4 Support (Decent and safe living and working conditions; career advancement opportunities; social recognition measures; others)
England In September 2019, the Government announced a £210 million funding boost for frontline NHS staff which included a £1,000 personal development budget for every nurse, midwife, and allied health professional working in the NHS in England to support their continuing professional development. As mentioned at 4.3.1 the NHS People Plan sets out a range of actions to transform people’s day to day experience of working in the NHS, focusing on the things that matter to staff including support for their wellbeing, improving flexible working opportunities and building a supportive and inclusive workplace culture.
[q4x4x]
4.4 Other relevant measures
No
[q5]
5. Are there specific policies and/or laws that guides international recruitment, migration and integration of foreign-trained health personnel in your country?
Yes
[q5x1]
5.1 Please provide further information in the box below:
Law/policy 1
The Code of Practice for the International recruitment of health and social care personnel sets guiding principles and best practice benchmarks for recruiters to follow. The Code: o ensures international recruits will be treated fairly and be provided with the appropriate support, o provides safeguards against active recruitment from 47 countries on the WHO Health Workforce Support and Safeguards List; o sets out how the UK is supporting countries with the most pressing health and social care workforce challenges.
Law/policy 2
International health and care professionals are required to register with the relevant UK professional regulator to lawfully practise in the UK. These regulators have specific procedures in place to register international health and care professionals that ensures patient and public safety. In most cases, for an applicant to be successfully registered they must satisfy the regulator that they are sufficiently qualified, possess the appropriate knowledge, skills or experience to practise in the UK, and are of good health and character. These requirements are set by the regulators with the DHSC being responsible for maintaining the appropriate legislation and amendments.
Law/policy 3
In January 2021, the UK Government introduced a new points-based immigration system which reduces the salary and skills thresholds that international recruits need in order to get a working visa. Other improvements include linking salary thresholds to NHS pay-scales and streamlining the system by removal of the visa cap and resident labour market test. The Health and Care visa, introduced on 4 August 2020 has made it easier and quicker for those wishing to work in the health and care sector through reduced visa fees, a Home Office visa decision within three weeks and an exemption to the Immigration Health Surcharge for applicants and their families.
[q6x]
6. Recognizing the role of other government entities, does the Ministry of Health have processes (e.g. policies, mechanisms, unit) to monitor and coordinate across sectors on issues related to the international recruitment and migration of health personnel?
Yes
[q6x1]
6.1 Please provide further information in the box below:
The Cross-Whitehall International Recruitment Steering Group for Health brings together key Government Departments (including the Home Office, the Department for Trade and the Foreign Commonwealth and Development Office), the devolved administrations and key system partners (NHS Employers NHS EI and HEE) to provide national policy oversight and collaboration on international recruitment workforce supply.
The Steering Group has a role in monitoring information on migrant flows to understand where recruits have come from, with a particular focus on low to middle income countries and fragile and conflict-affected states. Where trends indicate recruitment activity from low and lower middle-income countries or fragile and conflict-affected states, further work may take place to understand the cause and impact of this activity.
[q7x]
7. Has your country established a database or compilation of laws and regulations related to international health personnel recruitment and migration and, as appropriate, information related to their implementation?
No
Responsibilities, Rights and Recruitment Practices
[q8x]
8. Which legal safeguards and/or other mechanisms are in place to ensure that migrant health personnel enjoy the same legal rights and responsibilities as the domestically trained health workforce? Please tick all options that apply from the list below:
8.1 Migrant health personnel are recruited internationally using mechanisms that allow them to assess the benefits and risk associated with employment positions and to make timely and informed decisions regarding them
8.2 Migrant health personnel are hired, promoted and remunerated based on objective criteria such as levels of qualification, years of experience and degrees of professional responsibility on the same basis as the domestically trained health workforce
8.3 Migrant health personnel enjoy the same opportunities as the domestically trained health workforce to strengthen their professional education, qualifications and career progression
8.4 Other mechanisms, please provide details below if possible:
[q8xoth]
8.4 Please describe at least one mechanism
Mechanism 1
A guiding principle of the UK Code of Practice is that international health and social care personnel will have the same legal rights and responsibilities as domestically trained staff in all terms of employment and conditions of work. They will also have the same access to further education and training and continuous professional development. The 13 best practice benchmarks outline specific actions that employers and agencies should take to achieve this. It is expected that all organisations that comply with the code will apply these best practice benchmarks and will enter into contracts solely with recruitment agencies that have also agreed to abide by these.
Mechanism 2
The international recruitment framework ensures compliance with NHS pre-employment standards and grants access to a wide range of experienced international recruitment organisations, all of which operate at a high standard of quality. Agencies on the framework have also signed up to the Code of Practice.
Mechanism 3
[q9x]
9. Please submit any other comments or information you wish to provide regarding legal, administrative and other measures that have been taken or are planned in your country to ensure fair recruitment and employment practices of foreign-trained and/or immigrant health personnel.
The NHS Employers International Recruitment Toolkit has been produced to support NHS staff who are leading and delivering international recruitment. It aims to encourage and enable supportive practices and processes for the recruitment of international staff across a wide range of professions. It sets out in more detail the personal and professional support international recruits will require to get settled in the UK and to adjust to the cultural and working differences of the NHS. The toolkit is updated regularly and includes a dedicated component on continuing international recruitment during COVID-19 .
The Guide for International nurses during COVID-19 was created by NHS England and NHS Improvement, with the support of NHS Employers and the unions to provide a collection of national resources and guidance to support international nurses during the COVID-19 pandemic.
Diaspora Groups
NHS England and Improvement has been working with international nursing associations to enhance the overall pastoral support to overseas nurses. This includes sharing of best practice and initiatives, discussion of common challenges, particularly during COVID-19, and supporting new groups to get up and running.
Links to 16 International Nursing Associations is provided on page 66 of the International Recruitment Toolkit.
[q10x]
10. Regarding domestically trained/ emigrant health personnel (diaspora) working outside your country, please submit any comments or information on measures that have been taken or are planned in your country to ensure their fair recruitment and employment practices, as well as difficulties encountered
Measure 1
N/A
Measure 2
Measure 3
Data on International Health Personnel Recruitment & Migration
[iq11]
Improving the availability and international comparability of data is essential to understanding and addressing the global dynamic of health worker migration.
[q11]
11. Does your country have any mechanism(s) or entity(ies) to maintain statistical records of foreign-born and foreign-trained health personnel?
Yes
[q11x1]
Please describe
NHS Electronic Staff Record (ESR) – it provides self-reported nationality data for anyone working in the NHS, on a quarterly basis
Professional Regulator reports (NMC and GMC) – These count anyone who joins the UK register who originally qualified and registered overseas. This is cross-UK and includes NHS and independent settings
The full GMC and NMC registrant joiner and stock datasets are provided in Annex A.
[iQ12]
12. Data on the active stock of health personnel, disaggregated by country of training and birth
Previous data shared with WHO is available here. Please liaise with your NHWA focal point and update as relevant.
For the latest year available, consistent with the National Health Workforce Accounts (NHWA) Indicators 1-07 and 1-08, please provide information on the total stock of health personnel in your country (preferably the active workforce1), disaggregated by the country of training (foreign-trained) and the country of birth (foreign-born). Please consult with your NHWA focal point, if available, to ensure that data reported below is consistent with NHWA reporting.
Previous data shared with WHO is available here. Please liaise with your NHWA focal point and update as relevant.
For the latest year available, consistent with the National Health Workforce Accounts (NHWA) Indicators 1-07 and 1-08, please provide information on the total stock of health personnel in your country (preferably the active workforce1), disaggregated by the country of training (foreign-trained) and the country of birth (foreign-born). Please consult with your NHWA focal point, if available, to ensure that data reported below is consistent with NHWA reporting.
[q12x0]
12.1 Consolidated stock of active health personnel
This information can be provided by one of the following three options. Please choose your preferred mode of data entry:
This information can be provided by one of the following three options. Please choose your preferred mode of data entry:
Option B: Download the Excel template with existing data and Upload with the updated data
No comment
[q12x1x3]
Upload any format of documentation that provides such information (e.g. pdf, excel, word).
No comment
[q13x2]
12.2 Top 10 countries of training for foreign-trained health personnel
Please provide data on the top 10 countries of training for foreign-trained health personnel in your country. This information can be provided by one of the following two options:
Please provide data on the top 10 countries of training for foreign-trained health personnel in your country. This information can be provided by one of the following two options:
Option B: Download the Excel template with existing data and Upload with the updated data
[q13x2x2]
Option B: Completion of the template in Excel
Download and Upload
Download and Upload
Please upload file (Maximum file size: 5MB)
[q13x2x3]
Upload any format of documentation that provides such information (e.g. pdf, excel, word).
Please upload file
No comment
COVID-19 and Health personnel mobility
[q13]
13. Were measures undertaken at national or sub-national level in response to the COVID-19 pandemic with respect to the temporary or permanent mobility of international health personnel?
13.1 No change in national or sub-national regulation, policy or processes related to the entry or exit of foreign-trained or foreign-born health personnel
13.2 National and/or sub-national regulation, policy or processes enacted to ease entry and integration of foreign-trained or foreign-born health personnel
The Government and its NHS partners have proactively provided a wide range of measures to the NHS workforce during the COVID-19 pandemic: • Emergency legislation was passed to create a temporary ‘emergency’ register of healthcare professionals – 47,000 former health professionals joined this register and made themselves available to support the NHS and vaccination programme. • Temporary measures introduced to extend the visas of all regulated healthcare professionals across the NHS and the independent sector during the COVID-19 outbreak, with the latest 12-month extension to cover those whose visas were due to expire before 1 October 2021. • Arrangements were put in place to enable healthcare students to graduate early or take up paid clinical placements. • A national package of support for staff wellbeing was put in place and has been well received by staff in the NHS. This was bolstered by many initiatives led by local employers. • The health and safety of staff has been prioritised, ensuring access to PPE, testing and putting in place risk assessments to address the disproportionate impact of COVID-19 on some groups of NHS staff, most notably the ethnic minority workforce. • The families and dependents of international NHS support staff and social care workers who die as result of contracting coronavirus are offered the right of indefinite leave to remain in the UK.
13.3 National and/or sub-national regulation, policy or processes enacted to limit the exit of health personnel from country
13.4 Others
[q14]
14. Did you have a mechanism to monitor the inflow and outflow of health personnel to/from your country during the COVID-19 pandemic?
Inflow
Outflow
No
[q14x1]
14.1 How many foreign-trained or foreign-born health personnel were newly (inflow) active (temporarily and/or permanently) in your country in 2019 and 2020?
| Doctors | Nurses | Midwives | Dentists | Pharmacists | Comments | |
|---|---|---|---|---|---|---|
|
Data Source (e.g. Regulatory authority, immigration records, work permits, etc.) Please ensure data source consistency for each category of personnel for the two years |
||||||
| 2020 | 9780 | 6535 | ||||
| 2019 | 11020 | 10791 |
[q15]
15. Please list any challenges related to ethical international recruitment of health personnel during the COVID-19 pandemic
Please describe (e.g. active recruitment of ICU personnel)
Please describe (e.g. active recruitment of ICU personnel)
1st Challenge
Please describe (e.g. active recruitment of ICU personnel) Disruption to travel for international nurses and at times a ban on international travel in response to COVID-19 e.g: - Twice in 2020 the Philippines stopped the departure of internationally recruited nurses for some weeks so they could be deployed in the Filipino health system. - In May 2021, due to the huge upsurge of COVID-19 cases in India the UK temporarily paused the travel of nurses recruited from India.
2nd Challenge
3rd Challenge
Constraints, Solutions, and Complementary Comments
[q16]
16. Please list in priority order, the three main constraints to the ethical management of international migration in your country and propose possible solutions
| Main constraints | Possible solution /Recommendation | |
|---|---|---|
| 16.1a There are high levels of passive recruitment from countries on the WHO Health Workforce Support and Safeguards list e.g. Nigeria, this requires management whilst recognising the need to protect an individual’s right to migrate. | 16.1b Governments of countries with high levels of outward passive migration should consider what measures they can put in place to regulate recruitment activity in their country and to ensure the benefits associated with outward migration are maximised. The UK Government is keen to support this through the development of Government to Government bilateral agreements to set parameters for migration and the nature of UK support to ensure recruitment does not exacerbate existing domestic workforce shortages in the country of origin and mutual benefits are obtained. | |
| 16.2a There is no single, robust data UK source, to monitor health and care workforce migration inflows to ensure implementation of a Code of Practice for international recruitment is having the intended effects. | 16.2b The Cross Whitehall International Recruitment Steering Group has a role to monitor national migration flows to understand where recruits have come from, with a particular focus on low to middle income countries and fragile and conflict-affected states. A range of data sets will be considered by the Steering Group to set a baseline and this will be considered on a triannual basis to monitor changes in migration flows. New possible data sources are also being investigated to strengthen the available evidence base. | |
| 16.3a There are limited levers to ensure independent sector health and social care organisations abide by the UK Code of Practice and use agencies on the NHS Employers managed agency list. | 16.3b This is managed through wide publicization of the Code of Practice and ensuring it is understood by recruiters working in both sectors and is viewed as best practice. The UK Code will be reviewed and updated one year after publication which will provide an opportunity to strengthen implementation of the Code and re-promote it across the public and private sectors |
[q17]
17. Is there any specific support your country requires to strengthen implementation of the Code?
17.1 Support to strengthen data and information
17.2 Support for policy dialogue and development
17.3 Support for the development of bilateral/multi-lateral agreements
17.4 Other areas of support:
[q18]
18. Submit any other complementary comments or material you may wish to provide regarding the international recruitment and migration of health personnel, as related to implementation of the Code.
[q18x1]
Please upload any supporting files
Thank You
[iThank]
You have reached the end of the National Reporting Instrument - 2021. You may go back to any question to update your answers or confirm your entry by clicking ‘Submit’.