National Reporting Instrument 2024
Background
Adopted in 2010 at the 63rd World Health Assembly (WHA Res 63.16), the WHO Global Code of Practice on the International Recruitment of Health Personnel (“the Code”) seeks to strengthen the understanding and ethical management of international health personnel recruitment through improved data, information, and international cooperation.
Article 7 of the Code encourages WHO Member States to exchange information on the international recruitment and migration of health personnel. The WHO Director General is mandated to report to the World Health Assembly every 3 years.
WHO Member States completed the 4th round of national reporting in May 2022. The WHO Director General reported progress on implementation to the 75th World Health Assembly in May 2022 (A75/14). The report on the fourth round highlighted the need to assess implications of health personnel emigration in the context of additional vulnerabilities brought about by the COVID-19 pandemic. For this purpose, the Expert Advisory Group on the relevance and effectiveness of the Code (A 73/9) was reconvened. Following the recommendations of the Expert Advisory Group, the Secretariat has published the WHO health workforce support and safeguards list 2023.
The National Reporting Instrument (NRI) is a country-based, self-assessment tool for information exchange and Code monitoring. The NRI enables WHO to collect and share current evidence and information on the international recruitment and migration of health personnel. The findings from the 5th round of national reporting will be presented to the Executive Board (EB156) in January 2025 in preparation for the 78th World Health Assembly.
The deadline for submitting reports is 31 August 2024.
Article 9 of the Code mandates the WHO Director General to periodically report to the World Health Assembly on the review of the Code’s effectiveness in achieving its stated objectives and suggestions for its improvement. In 2024 a Member-State led expert advisory group will be convened for the third review of the Code’s relevance and effectiveness. The final report of the review will be presented to the 78th World Health Assembly.
For any queries or clarifications on filling in the online questionnaire please contact us at WHOGlobalCode@who.int.
What is the WHO Global Code of Practice?
Disclaimer: The data and information collected through the National Reporting Instrument will be made publicly available via the NRI database (https://www.who.int/teams/health-workforce/migration/practice/reports-database) following the proceedings of the 78th World Health Assembly. The quantitative data will be used to inform the National Health Workforce Accounts data portal (http://www.apps.who.int/nhwaportal/).
Disclaimer
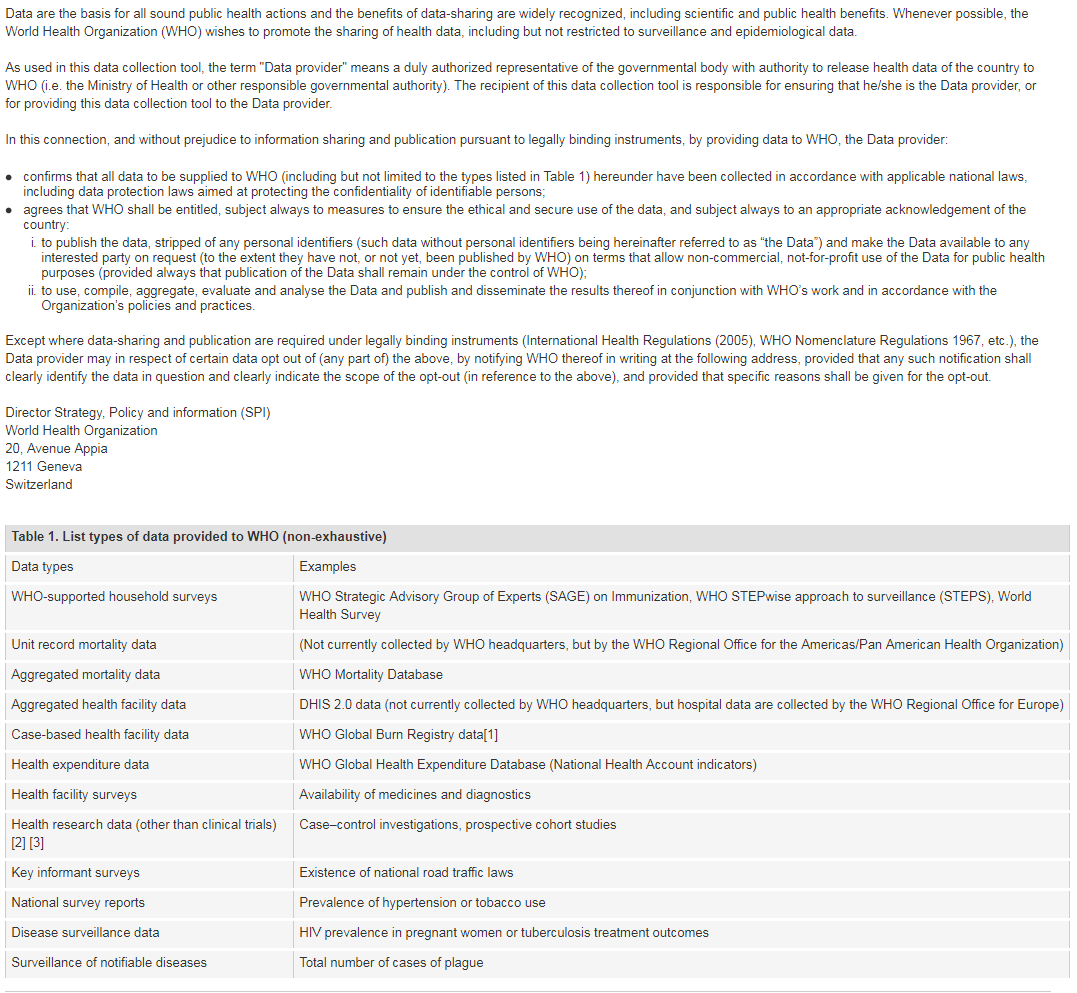
[1] Note: Case-based facility data collection as that in the WHO Global Bum Registry does not require WHO Member State approval.
[2] The world health report 2013: research for universal coverage. Geneva: World Health Organization; 2013 (http://apps.who.int/iris/bitstream/10665/85761/2/9789240690837_eng.pdf)
[3] WHO statement on public disclosure of clinical trial results: Geneva: World Health Organization; 2015 (http://www.who.int/ictrp/results/en/, accessed 21 February 2018).
For more information on WHO Data Policy kindly refer to http://www.who.int/publishing/datapolicy/en/
Contact Details
Contemporary issues
The UK continues to be a popular destination country choice for internationally mobile health and social care professionals and there has been a significant growth in the numbers of internationally trained doctors, nurses and care workers joining the workforce over the last three years. NHS Internationally trained staff have been part of the NHS since its inception in 1948. Over the past three years the NHS reliance on international recruitment to fill vacancies has increased. Latest professional regulator data shows that half of newly registered nurses in the UK and almost two thirds of newly licenced doctors are coming from overseas. This has been because of a combination of factors, including: - Focussed national efforts to build international recruitment capability and capacity within employers specifically to deliver the International Recruitment of Nurses Programme to contribute to the previous government’s commitment to increase the number of nurses working in the NHS by 50,000 (England). - All-Wales International Recruitment programme has been running since 2022, recruiting over 1,000 internationally educated healthcare professionals to date (Wales) - An International Recruitment project for nurses has been in place in Northern Ireland since 2016 with more than 1,670 nurses recruited in total and 973 of these being recruited in the last three years. (Northern Ireland) - In Scotland, the international recruitment of Nurses, Midwives and Allied Health Professionals has been taking place since 2021 with well over 1,100 recruits in posts across Health Boards. - Exemptions and simplifications in the visa process to make it cheaper and quicker for health and care staff to get visas than any other profession (UK wide) - Streamlined Nursing and Midwifery Council (NMC) regulatory processes (UK wide) Health and Care Worker visa data shows significant growth in visas granted between 2021 and 2022 with growth slowing in 2023. There were 19,842 nurse visas granted in 2021 increasing to 25,267 in 2022, reducing to 21,897 in 2023. For doctors, there were 5,775 visas granted in 2021, growing to 8,489 in 2022 and 8,832 in 2023. Looking forwards, the NHS Long Term Workforce Plan (published in 30 June 2023 under the previous Government) sets out how investment in domestic education and training will support the NHS to become less reliant on international recruitment for workforce supply in the medium to long term. However, international recruitment will continue to form an important part of our workforce, balanced against expanded domestic routes of supply (such as apprenticeships and traditional degree routes) and improved rates of retention. Adult Social Care (ASC) Growth in the international adult social care workforce was made possible following changes to the immigration system in 2022, making senior care workers and care workers eligible for the Health and Care Worker Visa. Latest data from Skills for Care shows that in year ending March 2024 there were 1.705 million filled posts in the adult social care sector, an increase of 4.2% (70,000 posts) from year ending March 2023. Skills for Care monthly indicative data shows continued improvement since then. It is likely that this overall growth depended on international recruitment with 105,000 recruits into care worker or senior care worker roles in 2023/24. In addition, there are ongoing challenges with domestic recruitment with Skills for Care data showing the number of posts in adult social care filled by people with a British nationality in 2023/24 decreasing by 70,000 since 2021/22 (-40,000 in 22/23 and –30,000 in 23/24) It is clear, international recruitment has played a valuable role in helping grow the adult social care workforce. It gives the health and care sectors the benefit of the skill and commitment of overseas workers who wish to work in England. During 2024 there have been several changes to the immigration system. Whilst the visa route for healthcare workers remained largely unaffected by the changes, there were specific changes to the care worker and senior care worker routes. In England, international recruitment of care workers and senior care workers is restricted to providers regulated by the Care Quality Commission. From March 11th 2024, care workers and senior care workers have no longer been able to bring dependants to the UK. Alongside these changes, UK Visas and Immigration implemented operational changes to strengthen controls to make sure only legitimate care providers with appropriate vacancies were able to recruit internationally. This is one of a number of factors which may have impacted visa application volumes. Data from the Home Office shows the number of health and care visas for care and senior care workers has decreased, with 3,300 visas granted in quarter one of 2024 compared with an average of 26,000 per quarter throughout 2023: Why do people come to the UK? To work - GOV.UK (www.gov.uk) The government recognises the scale of reforms needed to make the adult social care sector attractive, to support sustainable workforce growth and reduce the reliance on international recruitment. We want it to be regarded as a profession, and for the people who work in care to be respected as professionals. The government has set out a clear plan to bring down legal migration. The government’s new joined-up approach will see the newly formed Skills England, the Labour Market Advisory Board, and the Industrial Strategy Council work closely together with the independent Migration Advisory Committee to support and develop a structured and evidence-based approach to skills, migration, and labour market policy. This will reduce the need for international recruitment and ensure businesses are recruiting primarily from the homegrown workforce, boosting economic growth and providing quick responses to labour market changes. This approach will form a core part of the new government’s growth mission, supporting key industries in the process. Ethics The UK maintains a strong ethical approach to international recruitment. The Code of Practice for International Recruitment which promotes effective, fair and sustainable international recruitment practices. It is updated regularly as required and the Code red list – countries where active international recruitment is prohibited – is aligned with the latest WHO Health Workforce Support and Safeguards List. There is an Ethical Recruiters List of agencies and other recruiting organisations who have committed their adherence to the Code. We conduct regular checks of recruiters on this list, through NHS Employers, to ensure no proactive recruitment is taking place from red list countries and we are confident in this system. Following the WHO Global Code, our Code balances our duty to protect the most vulnerable health systems against the right of individuals to choose to migrate. Individuals in red list countries can therefore apply for UK vacancies if they do so directly and of their own accord. We know that the proportion of direct applications from red list countries is high. This is a concern for us. We know that people who migrate without support are at greater risk of exploitation, and we do not wish to deplete vulnerable countries of their health and care staff. However, domestic equality legislation enshrines the right for people to be treated equally during recruitment processes, regardless of where they are from. We have published guidance to address the risks facing international candidates with regards to scams and workplace exploitation when seeking a health or care job in the UK. The guidance ensures prospective candidates are well informed about the international recruitment process, benefits and challenges of seeking a health or care job in the UK. The guidance raises awareness of scams, sets out working rights and standards, details how to identify and deal with exploitation and signposts to further help or support. The guidance is published alongside an easy read leaflet which aims to engage international candidates and summarise the key messages. We are working with Foreign, Commonwealth and Development Office (FCDO) in-country health advisors and diaspora organisations to ensure the guidance is disseminated widely and reaches potential international candidates before they have taken the decision to move to the UK.
We are conscious of the attraction of other health economies trying to attract UK trained staff. This is something we are continuing to monitor, while also improving working conditions for NHS staff and competitive pay offers. More information about this is provided in the answer to question 2.2.3.
Health Personnel Education
Check all items that apply from the list below:
sectors on the international recruitment and migration of health personnel, as well as to publicize the Code, among relevant ministries, departments and agencies,
nationally and/or sub-nationally.
processes and/or involve them in activities related to the international recruitment of health personnel.
personnel authorized by competent authorities to operate within their jurisdiction.
Government Agreements
| a. Title of Agreement | b. Type of Agreement | |
|---|---|---|
| Agreement 1 | Memorandum of Understanding between the UK and Nepal on the recruitment of health workers | 1 |
| Agreement 2 | Bilateral Agreement Between the Government of the Republic of Kenya and the Government of the United Kingdom and Northern Ireland for collaboration Health Care Workforce | 1 |
| Agreement 3 | Memorandum of Understanding Between the Government of the Republic of the Philippines and the Government of the United Kingdom of Great Britain and Northern Ireland on Healthcare Cooperation | 1 |
| Agreement 4 | Memorandum of understanding between the UK and Sri Lanka on healthcare cooperation | 1 |
| Agreement 5 | Memorandum of understanding between the Government of Malaysia and the UK of Great Britain and Northern Ireland on Healthcare Cooperation | 1 |
| Agreement 6 | UK and India collaboration on healthcare workforce framework agreement | 1 |
| Agreement 7 | Memorandum of Understanding between the Welsh Government and Norka Roots (Government of Kerala) | 1 |
| Agreement 8 | EU Exit Standstill Provisions | 2 |
| Agreement 9 | Free trade agreement between Iceland, the Principality of Liechtenstein and the Kingdom of Norway and the United Kingdom of Great Britain and Northern Ireland | 2 |
| Agreement 10 | Agreement between the Swiss Confederation (Switzerland) and the UK on the Recognition of Professional Qualifications | 1 |
| Agreement 11 | ||
| Agreement 12 | ||
| Agreement 13 | ||
| Agreement 14 | ||
| Agreement 15 |
Government Agreements - 6.1 A
| Education and training | Health cooperation | Promotion of circular migration | Philanthropy or technical support | Qualification recognition | Recruitment of health personnel | Trade in services | Others | |
|---|---|---|---|---|---|---|---|---|
| Memorandum of Understanding between the UK and Nepal on the recruitment of health workers | 1 | |||||||
| Bilateral Agreement Between the Government of the Republic of Kenya and the Government of the United Kingdom and Northern Ireland for collaboration Health Care Workforce | 1 | |||||||
| Memorandum of Understanding Between the Government of the Republic of the Philippines and the Government of the United Kingdom of Great Britain and Northern Ireland on Healthcare Cooperation | 1 | |||||||
| Memorandum of understanding between the UK and Sri Lanka on healthcare cooperation | 1 | |||||||
| Memorandum of understanding between the Government of Malaysia and the UK of Great Britain and Northern Ireland on Healthcare Cooperation | 1 | |||||||
| UK and India collaboration on healthcare workforce framework agreement | 1 | 1 | 1 | |||||
| Memorandum of Understanding between the Welsh Government and Norka Roots (Government of Kerala) | 1 | |||||||
| EU Exit Standstill Provisions | 1 | |||||||
| Free trade agreement between Iceland, the Principality of Liechtenstein and the Kingdom of Norway and the United Kingdom of Great Britain and Northern Ireland | 1 | |||||||
| Agreement between the Swiss Confederation (Switzerland) and the UK on the Recognition of Professional Qualifications | 1 | |||||||
| Doctors | Nurses | Midwives | Dentists | Pharmacists | Other occupations | |
|---|---|---|---|---|---|---|
| Memorandum of Understanding between the UK and Nepal on the recruitment of health workers | 1 | 1 | 1 | 1 | 1 | |
| Bilateral Agreement Between the Government of the Republic of Kenya and the Government of the United Kingdom and Northern Ireland for collaboration Health Care Workforce | 1 | |||||
| Memorandum of Understanding Between the Government of the Republic of the Philippines and the Government of the United Kingdom of Great Britain and Northern Ireland on Healthcare Cooperation | 1 | 1 | ||||
| Memorandum of understanding between the UK and Sri Lanka on healthcare cooperation | 1 | 1 | 1 | |||
| Memorandum of understanding between the Government of Malaysia and the UK of Great Britain and Northern Ireland on Healthcare Cooperation | 1 | 1 | 1 | 1 | ||
| UK and India collaboration on healthcare workforce framework agreement | 1 | 1 | ||||
| Memorandum of Understanding between the Welsh Government and Norka Roots (Government of Kerala) | 1 | 1 | 1 | |||
| EU Exit Standstill Provisions | 1 | 1 | 1 | 1 | 1 | |
| Free trade agreement between Iceland, the Principality of Liechtenstein and the Kingdom of Norway and the United Kingdom of Great Britain and Northern Ireland | 1 | 1 | 1 | 1 | 1 | 1 |
| Agreement between the Swiss Confederation (Switzerland) and the UK on the Recognition of Professional Qualifications | 1 | 1 | 1 | 1 | 1 | 1 |
| Start Year | End Year | |
|---|---|---|
| Memorandum of Understanding between the UK and Nepal on the recruitment of health workers | 2023 | 2028 |
| Bilateral Agreement Between the Government of the Republic of Kenya and the Government of the United Kingdom and Northern Ireland for collaboration Health Care Workforce | 2021 | Remain in force unless it is terminated by either party giving 1 year notice |
| Memorandum of Understanding Between the Government of the Republic of the Philippines and the Government of the United Kingdom of Great Britain and Northern Ireland on Healthcare Cooperation | 2021 | For 3 years and will be automatically extended for the same period unless one participant notifies the other of desire to suspend of terminate |
| Memorandum of understanding between the UK and Sri Lanka on healthcare cooperation | 2022 | for 4 years and automatically renewed for similar period unless either party notifies intention to terminate |
| Memorandum of understanding between the Government of Malaysia and the UK of Great Britain and Northern Ireland on Healthcare Cooperation | 2021 | for 5 years and renewed for a further 5 years unless otherwise decided by the participants |
| UK and India collaboration on healthcare workforce framework agreement | 2022 | remains effected until terminated – with 1 years written notice of intention to terminate |
| Memorandum of Understanding between the Welsh Government and Norka Roots (Government of Kerala) | 2024 | 2026 |
| EU Exit Standstill Provisions | 2021 | N/A |
| Free trade agreement between Iceland, the Principality of Liechtenstein and the Kingdom of Norway and the United Kingdom of Great Britain and Northern Ireland | 2023 | N/A |
| Agreement between the Swiss Confederation (Switzerland) and the UK on the Recognition of Professional Qualifications | 2025 | N/A |
benefit the health system of my country and partner country(ies)
benefit the health system of my country and partner country(ies)
benefit the health system of my country and partner country(ies)
benefit the health system of my country and partner country(ies)
benefit the health system of my country and partner country(ies)
benefit the health system of my country and partner country(ies)
benefit the health system of my country and partner country(ies)
benefit the health system of my country and partner country(ies)
benefit the health system of my country and partner country(ies)
benefit the health system of my country and partner country(ies)
Government Agreements - 6.1 B
| Start year of implementation: | |
|---|---|
| Memorandum of Understanding between the UK and Nepal on the recruitment of health workers | 2023 |
| Bilateral Agreement Between the Government of the Republic of Kenya and the Government of the United Kingdom and Northern Ireland for collaboration Health Care Workforce | |
| Memorandum of Understanding Between the Government of the Republic of the Philippines and the Government of the United Kingdom of Great Britain and Northern Ireland on Healthcare Cooperation | |
| Memorandum of understanding between the UK and Sri Lanka on healthcare cooperation | |
| Memorandum of understanding between the Government of Malaysia and the UK of Great Britain and Northern Ireland on Healthcare Cooperation | |
| UK and India collaboration on healthcare workforce framework agreement | |
| Memorandum of Understanding between the Welsh Government and Norka Roots (Government of Kerala) | |
| EU Exit Standstill Provisions | 2021 |
| Free trade agreement between Iceland, the Principality of Liechtenstein and the Kingdom of Norway and the United Kingdom of Great Britain and Northern Ireland | 2023 |
| Agreement between the Swiss Confederation (Switzerland) and the UK on the Recognition of Professional Qualifications | |
Agreement: Memorandum of Understanding between the UK and Nepal on the recruitment of health workers
| Number of personnel | |
|---|---|
| Doctors | 0 |
| Nurses | 41 |
| Midwives | 0 |
| Dentists | 0 |
| Pharmacists | 0 |
Agreement: EU Exit Standstill Provisions
| Number of personnel | |
|---|---|
| Doctors | See annex A |
| Nurses | See annex A |
| Midwives | See annex A |
| Dentists | Not available |
| Pharmacists | Not available |
Agreement: Free trade agreement between Iceland, the Principality of Liechtenstein and the Kingdom of Norway and the United Kingdom of Great Britain and Northern Ireland
| Number of personnel | |
|---|---|
| Doctors | Not available |
| Nurses | Not available |
| Midwives | Not available |
| Dentists | Not available |
| Pharmacists | Not available |
| all professions regulated in law | Not available |
| Upload document(s) | |
|---|---|
| Memorandum of Understanding between the UK and Nepal on the recruitment of health workers | |
| Bilateral Agreement Between the Government of the Republic of Kenya and the Government of the United Kingdom and Northern Ireland for collaboration Health Care Workforce | |
| Memorandum of Understanding Between the Government of the Republic of the Philippines and the Government of the United Kingdom of Great Britain and Northern Ireland on Healthcare Cooperation | |
| Memorandum of understanding between the UK and Sri Lanka on healthcare cooperation | |
| Memorandum of understanding between the Government of Malaysia and the UK of Great Britain and Northern Ireland on Healthcare Cooperation | |
| UK and India collaboration on healthcare workforce framework agreement | |
| Memorandum of Understanding between the Welsh Government and Norka Roots (Government of Kerala) | |
| EU Exit Standstill Provisions | |
| Free trade agreement between Iceland, the Principality of Liechtenstein and the Kingdom of Norway and the United Kingdom of Great Britain and Northern Ireland | |
| Agreement between the Swiss Confederation (Switzerland) and the UK on the Recognition of Professional Qualifications | |
Responsibilities, rights and recruitment practices
Please check all items that apply from the list below:
Please check all items that apply from the list below:
International migration
| Direct (individual) application for education, employment, trade, immigration or entry in country |
Government to government agreements that allow health personnel mobility |
Private recruitment agencies or employer facilitated recruitment |
Private education/ immigration consultancies facilitated mobility |
Other pathways (please specify) | Which pathway is used the most? Please include quantitative data if available. | |
|---|---|---|---|---|---|---|
| Doctors | 1 | 1 | 1 | 0 | ||
| Nurses | 1 | 1 | 1 | 0 | ||
| Midwives | 1 | 1 | 1 | 0 | ||
| Dentists | 1 | 1 | 1 | 0 | ||
| Pharmacists | 1 | 1 | 1 | 0 | ||
| Other occupations | 0 | 0 | 0 | 0 | ||
| Other occupations | 0 | 0 | 0 | 0 | ||
| Other occupations | 0 | 0 | 0 | 0 | ||
| Other occupations | 0 | 0 | 0 | 0 | ||
| Other occupations | 0 | 0 | 0 | 0 |
| Direct (individual) application for education, employment, trade, immigration, or entry in the destination country |
Government to government agreements that allow health personnel mobility |
Private recruitment agencies or employer facilitated recruitment |
Private education/ immigration consultancies facilitated mobility |
Other pathways (please specify) | Which pathway is used the most? Please include quantitative data if available. | |
|---|---|---|---|---|---|---|
| Doctors | 0 | 0 | 0 | 0 | ||
| Nurses | 0 | 0 | 0 | 0 | ||
| Midwives | 0 | 0 | 0 | 0 | ||
| Dentists | 0 | 0 | 0 | 0 | ||
| Pharmacists | 0 | 0 | 0 | 0 | ||
| Other occupations | 0 | 0 | 0 | 0 | ||
| Other occupations | 0 | 0 | 0 | 0 | ||
| Other occupations | 0 | 0 | 0 | 0 | ||
| Other occupations | 0 | 0 | 0 | 0 | ||
| Other occupations | 0 | 0 | 0 | 0 |
Recruitment & migration
Improving the availability and international comparability of data is essential to understanding and addressing the global dynamic of health worker migration. Please consult with your NHWA focal point, if available, to ensure that data reported below is consistent with NHWA reporting*.
(The list of NHWA focal points is available here. Please find the focal point(s) for your country from the list and consult with them.)
For countries reporting through the WHO-Euro/EuroStat/OECD Joint data collection process, please liaise with the JDC focal point.
Inflow and outflow of health personnel
| Doctors | Nurses | Midwives | Dentists | Pharmacists | Remarks | |
|---|---|---|---|---|---|---|
| 2021 | ||||||
| 2022 | ||||||
| 2023 | ||||||
| Data Source (e.g. Regulatory authority, immigration records, work permits, etc.) |
Stock of health personnel
For the latest year available, consistent with the National Health Workforce Accounts (NHWA) Indicators 1-07 and 1-08, please provide information on the total stock of health personnel in your country (preferably the active workforce), disaggregated by the place of training (foreign-trained) and the place of birth (foreign-born).
This information can be provided by one of the following two options:
Technical and financial support
| Country supported | Type of support (please specify) | |
|---|---|---|
| Somaliland, Uganda, Ghana 2021-2022 | 2021-2022 £5m Building the Future International Workforce (FIWP) funded by Official Development Assistance (ODA) supported: • health workforce planning and management • provided training opportunities for refugees/displaced people to find sustainable employment • linked NHS institutions with in-country health institutions to support education and retention | |
| Nigeria, Kenya, Ghana 2022-2025 | 2022-2025 £15m Global Health Workforce Programme (GHWP) funded by ODA awarded: • approx. £6m to WHO to support health workforce planning and employment and capacity-building work including training and retention, including £1m invested in the ILO-OECD-WHO Working for Health Multi-Partner Trust Fund. • approx. £9m to the Tropical Health and Education Trust (THET) to set up and coordinate health partnerships on retention and wellbeing strategies, training opportunities and improved quality of curriculum, policies, and regulation | |
| Ghana, Malawi, Nepal and Philippines | 2023-2026 £2.93m FCDO UK (ODA) funded Health Systems Connect Programme. • In Ghana, a workstream is focussing on developing systems and structures to support the mental health of Ghana’s health workforce. • In Malawi, one workstream is focussing on Building a sustainable architecture for public health specialty training to strengthen the Public Health Specialty workforce. The other workstream is strengthening workforce planning and forecasting capability in Malawi. • In Nepal, a workstream is focussing on workforce planning transformation and management in Lumbini Province. In the Philippines, the NHSC is supporting the implementation and operationalization of a healthcare provider network, with a cross-cutting theme of workforce development and digital transformation. | |
| South Africa | 2022-2026 £680k British High Commission (ODA) funded UK-South Africa Health System Strengthening Partnership, focusses on workforce development for health technology assessment, medico legal and hospital governance and leadership. |
| Country supported | Type of support (please specify) | |
|---|---|---|
| Nigeria, Kenya, Ghana 2022-2025 | As part of the 2022-2025 £15m Global Health Workforce Programme (GHWP) • WHO offices supported administrative systems and capacity building of Human Resources for Health public policy stewardship, leadership and governance • THET supported partnerships on improved health workforce leadership capacity | |
| Lesotho, Zambia, South Africa, Uganda, Saint Vincent and the Grenadines, Thailand | Funded by NHS England, the NHS Global Fellowship Programme offers leadership development opportunities for clinical and non-clinical staff from the NHS to experience health systems across the globe. Fellows focus on either quality improvement or research co-developed with local and/or national partners to enhance the patient experience, improve health outcomes and reduce health inequalities. • Between 2019-2023, 13 NHS Global Fellows have undertaken projects in Lesotho. • Between 2018-2023, 24 NHS Global Fellows have undertaken projects in Zambia. • Between 2013-2023, 121 NHS Global Fellows have undertaken projects in South Africa. • Between 2020-2023, 14 NHS Global Fellows have undertaken projects in Uganda. • Between 2022-2023, 5 NHS Global Fellows have undertaken projects in Saint Vicent and the Grenadines. • Between 2022-2023, 10 NHS Global Fellows have undertaken projects in Thailand. | |
| Malawi 2018-25 (Scotland) | • Scotland Malawi Mental Health Education Project - £330k funding to support the “Consolidating Psychiatry Capacity Development in Malawi Project” strengthening capacity and institutional partnership initiatives between Scotland/Malawi in training psychiatrists at undergraduate and postgraduate level. • MalDent project - £1.3m to establish an undergraduate dental degree (BDS) programme within the Faculty of Medicine, University of Malawi, to train Malawian dentists for the delivery of a national health programme. • MalScot programme- £220k per annum to develop same day cervical cancer 'screen and treat' programmes, through local capacity building. | |
| To note that this list is not exhaustive, the UK provides elements of health system strengthening which includes workforce development in a huge range of areas | The UK provides Official Development Assistance (ODA) to reduce poverty, tackle instability and create prosperity in developing countries This includes support for the development of the health workforce and the implementation of national health workforce strategies. Channels of support include bilateral health programmes that directly support national governments or civil society partners with financing or technical collaboration in response to national health workforce challenges. This includes: • health workforce education and training • curriculum development • continuing professional development • qualification development • national workforce policy • strengthening related ministry of health policy and planning functions such as public financial management |
Constraints, Solutions, and Complementary Comments
| Main constraints | Possible solutions/recommendations | |
|---|---|---|
| 15.1a The Code is non-statutory guidance, so compliance by employers and agencies is voluntary, and there are increasing reports of exploitative recruitment and employment practices by agencies and/or employers not following the Code. | 15.1b We have published international candidate guidance and an easy read leaflet to help address this, by supporting candidates to be well informed, warned about the risks, and are armed with organisations to contact if they are in trouble. This has been disseminated through our stakeholders and engagement events. We have worked with FCDO in-country posts to make it available in locations international candidates may visit as part of their application for roles in the UK, for example visa application centres and English language exam centres | |
| 15.2a There are high levels of direct applications (passive recruitment) from countries on the WHO Health Workforce Support and Safeguards list e.g. Nigeria. However, domestic equality legislation enshrines the right for people to be treated equally during recruitment processes, regardless of where they are from, so options to manage this in the UK are limited. | 15.2b The NHS Employers managed Ethical Recruiters List – formally the Agency List - was widened in August 2022 to include any organisation which recruits on behalf of another organisation. This change meant any organisation which in effect is operating like a recruitment agency, follows the same rules as a recruitment agencies and cannot accept direct applications from red list countries. NHS England also undertook engagement activity to influence employers to move away from recruitment models which rely on direct applications. Governments of countries with high levels of outward passive migration should consider what measures they can put in place to regulate recruitment activity in their country and to ensure the benefits associated with outward migration are maximised. | |
| 15.3a There are limited levers to ensure independent sector health and social care organisations abide by the UK Code of Practice and use recruiting organisation on the NHS Employers managed Ethical Recruiters List. | 15.3b This is managed through wide publicization of the Code of Practice and ensuring it is understood by recruiters working in both sectors and is viewed as best practice. Whenever the UK Code is updated, it is re-promoted it across the public and private sectors and all organisations on the ethical recruiters list have to recommit to the updated Code in writing, otherwise they are removed from the list. In August 2022 a knowledge test was introduced to the Ethical Recruiters List application process to ensure all organisations appearing on the list fully understand the Code rules. |
The scope of the WHO Global Code of Practice should be expanded to include social care personnel. In the UK international recruitment has been vital to workforce supply in the social care sector. Many health professionals such as nurses and physiotherapists work in the social care sector, and the care worker role is one of the most straight forward ways for people to migrate to the UK as it requires low language and skill level. This has made it an attractive option for people from low-to-middle income countries, but also ripe for exploitation. In 2021 the UK Code of Practice was updated to include the social care sector, recognising that ethical international recruitment is just as important for workers in this sector. This needs to be recognised at a global level.
Please describe OR Upload (Maximum file size 10 MB)