National Reporting Instrument 2024
Background
Adopted in 2010 at the 63rd World Health Assembly (WHA Res 63.16), the WHO Global Code of Practice on the International Recruitment of Health Personnel (“the Code”) seeks to strengthen the understanding and ethical management of international health personnel recruitment through improved data, information, and international cooperation.
Article 7 of the Code encourages WHO Member States to exchange information on the international recruitment and migration of health personnel. The WHO Director General is mandated to report to the World Health Assembly every 3 years.
WHO Member States completed the 4th round of national reporting in May 2022. The WHO Director General reported progress on implementation to the 75th World Health Assembly in May 2022 (A75/14). The report on the fourth round highlighted the need to assess implications of health personnel emigration in the context of additional vulnerabilities brought about by the COVID-19 pandemic. For this purpose, the Expert Advisory Group on the relevance and effectiveness of the Code (A 73/9) was reconvened. Following the recommendations of the Expert Advisory Group, the Secretariat has published the WHO health workforce support and safeguards list 2023.
The National Reporting Instrument (NRI) is a country-based, self-assessment tool for information exchange and Code monitoring. The NRI enables WHO to collect and share current evidence and information on the international recruitment and migration of health personnel. The findings from the 5th round of national reporting will be presented to the Executive Board (EB156) in January 2025 in preparation for the 78th World Health Assembly.
The deadline for submitting reports is 31 August 2024.
Article 9 of the Code mandates the WHO Director General to periodically report to the World Health Assembly on the review of the Code’s effectiveness in achieving its stated objectives and suggestions for its improvement. In 2024 a Member-State led expert advisory group will be convened for the third review of the Code’s relevance and effectiveness. The final report of the review will be presented to the 78th World Health Assembly.
For any queries or clarifications on filling in the online questionnaire please contact us at WHOGlobalCode@who.int.
What is the WHO Global Code of Practice?
Disclaimer: The data and information collected through the National Reporting Instrument will be made publicly available via the NRI database (https://www.who.int/teams/health-workforce/migration/practice/reports-database) following the proceedings of the 78th World Health Assembly. The quantitative data will be used to inform the National Health Workforce Accounts data portal (http://www.apps.who.int/nhwaportal/).
Disclaimer
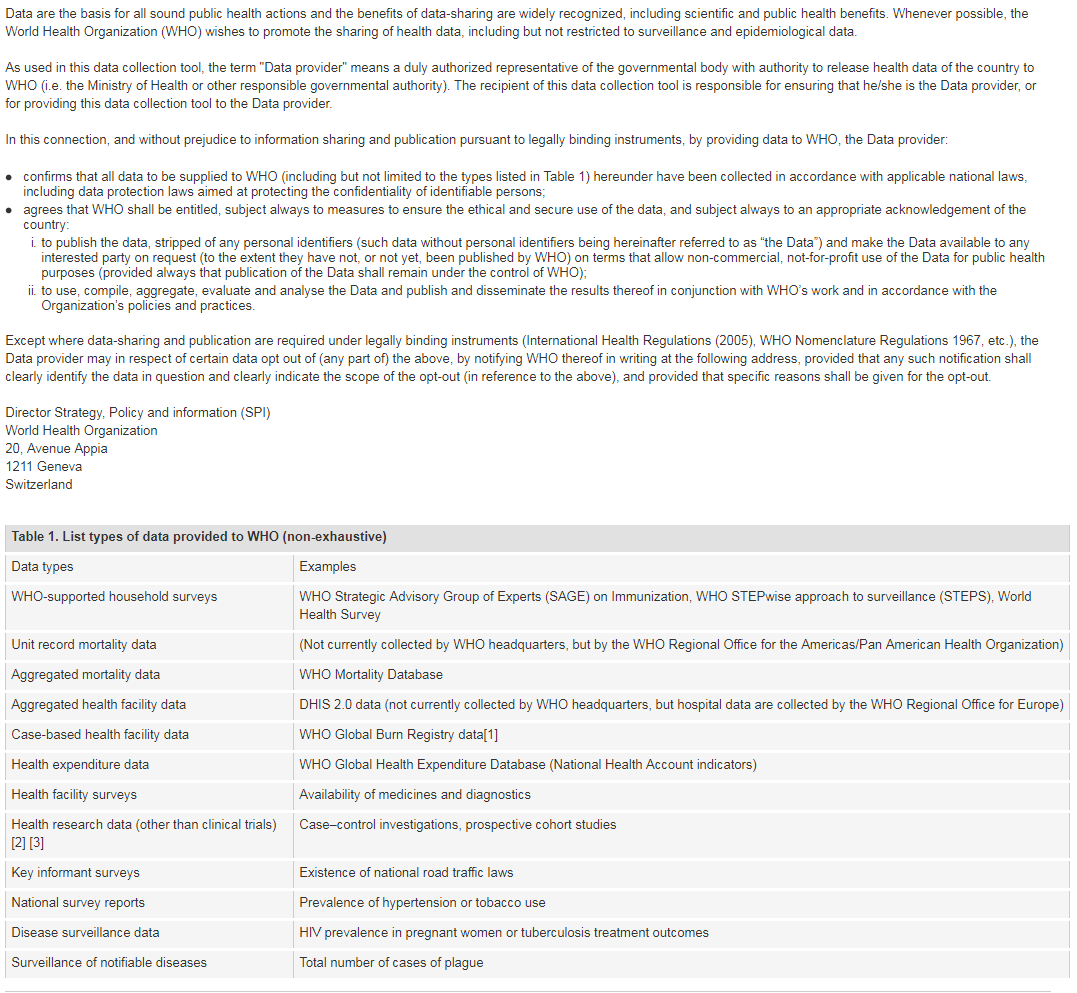
[1] Note: Case-based facility data collection as that in the WHO Global Bum Registry does not require WHO Member State approval.
[2] The world health report 2013: research for universal coverage. Geneva: World Health Organization; 2013 (http://apps.who.int/iris/bitstream/10665/85761/2/9789240690837_eng.pdf)
[3] WHO statement on public disclosure of clinical trial results: Geneva: World Health Organization; 2015 (http://www.who.int/ictrp/results/en/, accessed 21 February 2018).
For more information on WHO Data Policy kindly refer to http://www.who.int/publishing/datapolicy/en/
Contact Details
Contemporary issues
ISSUES - GENERAL: Ireland is a country with inward and outward migration of health and social care workers. The health services in Ireland operate in a competitive global market for skilled healthcare workers. There is significant demand for Irish healthcare internationally. - EMIGRATION: Ireland does not maintain a central register of those emigrating, however, there is evidence of increased mobility internationally (to other countries) of Irish registered/Irish trained professionals post pandemic. Research by the Central Statistics Office (CSO) and National Doctors Training Programme (NDTP) in the Health Service Executive (HSE) shows that a high proportion of emigrating doctors and nurses return to Ireland. - DOMESTIC STUDENTS STUDYING ABROAD: There are challenges with some Irish students studying abroad and not having the required competencies on return to gain registration. - ACCESS TO DOMESTIC STAFF: Stakeholders in the public and voluntary sector reported challenges accessing staff. Voluntary organisations also noted high care staff vacancy levels. - DOMESTIC SUPPLY: It takes many years to train new health and social care workers, recruiting them from abroad can provide a solution to address immediate shortages. - VISA PROCESS: Stakeholders reported that visa requirements can delay the recruitment process, as and a timeframe is required for processing. Some professions are not eligible for the Critical Skills Employment Permit - DATA: It is difficult to assess the scale of emigration as there is no central register, and for many professions, data on this is not currently collected by regulators. The country where workforce is emigrating from can at best capture “intent of emigration due to work” but this can only be captured by the countries these workforces are emigrating towards. MEASURES TO ADDRESS ISSUES - Ireland is seeking to improve self-sufficiency in accordance with our commitments under the WHO Global Code of Practice on the International Recruitment of Health Personnel. - BUILD STUDENT SUPPLY: Work is underway to expand the number of health and social care worker student places. - ATTRACT/ RETAIN EFFORTS: The Department of Health and the Health Service Executive work together to develop strategies that will positively impact recruitment and retention, including addressing issues such as workload, work–life balance, workplace culture, supportive management, career advancement and workplace safety. Examples of recently developed strategies that will be/are being implemented include the Health Service Executive (HSE) Resourcing Strategy, the Report of the Expert Review Body on Nursing and Midwifery, the Non-Consultant Hospital Doctor (NCHD) Taskforce Interim and Final Reports, the Report of the Strategic Workforce Advisory Group and Sharing the Vision. The primary pillar of the HSE Resourcing Strategy ‘Resourcing our Future’ is the retention of staff. From 2022 onwards there has been a steady increase in retention levels which is demonstrated by the recent turnover figures. This pattern is continuing in 2024. Within the Expert Review Body on Nursing and Midwifery, four recommendations are specifically focused on attracting, recruiting and retaining nurses and midwives and these recommendations are being led out by the HSE National HR Office as part of the implementation plan. - JOB OFFERS FOR GRADUATES: Retention of health care graduates has been at the forefront of resourcing for the public service over the last number of years, this has resulted in each HSCP and Nursing and Midwifery graduate getting offered permanent contracts of employment. In 2023 alone this has resulted in 83% of our nursing and midwifery graduates taking permanent positions in the publicly funded health services. Voluntary services also reported offering graduate positions/programmes. - EFFORTS TO ATTRACT DOMESTIC WORKERS TO IRELAND: The HSE works very closely with the regulators to attract both those trained in Ireland and overseas. An example of this was a partnership marketing campaign with CORU (regulator for Health & Social Care Professionals) to attract Irish applicants back to Ireland. - UNDERSTANDING MIGRATION PATTERNS: Recent research has been undertaken to better understand migration patterns. For example analysis by the Central Statistics Office on health graduates, and the National Doctors Training and Planning in the HSE on trainee doctors leaving the Irish health system and the numbers returning.
ISSUES - Feedback from across the sector reports a reliance on international recruitment of health personnel to meet domestic needs. - PROPORTION: The proportion of foreign trained doctors and nurses has been increasing over the past number of years. In 2023, 52% of nurses and 43% of doctors were foreign educated. The percentage of foreign trained doctors rose by 2.91% between 2021 and 2023. The percentage of foreign trained nurses rose by 5.28% between 2021 and 2023. - INCREASING RELIANCE: Stakeholders reported that there is increasing pressure to recruit from overseas across the public, private and voluntary sectors. This is due to a number of reasons including: o Increased investment in the public health service and the associated requirement to recruit additional staff. o Increased outflows of staff post pandemic to other jurisdictions. o Implementation of various policies that required additional staff. o Requirement to source some staff/professions from the international market that previously were available in the Irish labour market. - CHALLENGES ACCESSING STAFF: Public and voluntary organisations reported challenges accessing domestic staff. This can often result in vacancy rates and agency use. Voluntary organization stakeholders reported a greater chance of retaining international staff for longer periods as their work permits are tied to their employment thereby impacting their mobility within the domestic labour market. The costs of international recruitment were reported as better value for money than paying agency placement fees locally for staff who may be unlikely to retain in the longer term. However, under the Employment Permits Acts 2024, to be commenced in the coming weeks, subject to certain conditions, a permit holder may change to a similar role with a new employer for any reason, after a prescribed period of nine months. MEASURES TO ADDRESS ISSUES - Ireland is seeking to improve self-sufficiency in accordance with our commitments under the WHO Global Code of Practice on the International Recruitment of Health Personnel. - BUILD STUDENT SUPPLY: Work is underway to expand the number of health and social care worker student places. - EXPANDING ENTRY: The Department of Health and stakeholders are examining the scope to develop non-traditional career pathways, including expanded application of Apprenticeships and earn as your learn models The public health service is currently expanding the routes of entry to the register for some professions via the introduction of apprenticeships – commencing with social work in 2024. - INTERNATIONAL RECRUITMENT: International recruitment is carried out in line with the WHO Code of Practice. - MODELLING: There are modelling activities underway by the Department of Health, HSE and ESRI which provide projections of workforce demand and supply. Outputs from these modelling tools informs workforce planning activities.
Health Personnel Education
Check all items that apply from the list below:
sectors on the international recruitment and migration of health personnel, as well as to publicize the Code, among relevant ministries, departments and agencies,
nationally and/or sub-nationally.
processes and/or involve them in activities related to the international recruitment of health personnel.
personnel authorized by competent authorities to operate within their jurisdiction.
Government Agreements
| a. Title of Agreement | b. Type of Agreement | |
|---|---|---|
| Agreement 1 | Memorandum of Agreement Between The Queen’s University of Belfast And Minister for Further and Higher Education, Research, Innovation and Science Ireland And Minister for Health Ireland and Department of Health Northern Ireland | 1 |
| Agreement 2 | Memorandum of Understanding Between the Health Service Executive and with The College of Physicians and Surgeons Pakistan | 1 |
| Agreement 3 | Memorandum of Understanding Between the Health Service Executive andThe Sudan Medical & Specialisation Board (SMSB) | 1 |
| Agreement 4 | EU Directive 2005/36/EC;EU Directive 2013/55/EU; EU Directive 2018/958/EU | 2 |
| Agreement 5 | ||
| Agreement 6 | ||
| Agreement 7 | ||
| Agreement 8 | ||
| Agreement 9 | ||
| Agreement 10 | ||
| Agreement 11 | ||
| Agreement 12 | ||
| Agreement 13 | ||
| Agreement 14 | ||
| Agreement 15 |
Government Agreements - 6.1 A
| Education and training | Health cooperation | Promotion of circular migration | Philanthropy or technical support | Qualification recognition | Recruitment of health personnel | Trade in services | Others | |
|---|---|---|---|---|---|---|---|---|
| Memorandum of Agreement Between The Queen’s University of Belfast And Minister for Further and Higher Education, Research, Innovation and Science Ireland And Minister for Health Ireland and Department of Health Northern Ireland | 1 | |||||||
| Memorandum of Understanding Between the Health Service Executive and with The College of Physicians and Surgeons Pakistan | 1 | |||||||
| Memorandum of Understanding Between the Health Service Executive andThe Sudan Medical & Specialisation Board (SMSB) | 1 | |||||||
| EU Directive 2005/36/EC;EU Directive 2013/55/EU; EU Directive 2018/958/EU | 1 | |||||||
| Doctors | Nurses | Midwives | Dentists | Pharmacists | Other occupations | |
|---|---|---|---|---|---|---|
| Memorandum of Agreement Between The Queen’s University of Belfast And Minister for Further and Higher Education, Research, Innovation and Science Ireland And Minister for Health Ireland and Department of Health Northern Ireland | 1 | |||||
| Memorandum of Understanding Between the Health Service Executive and with The College of Physicians and Surgeons Pakistan | 1 | |||||
| Memorandum of Understanding Between the Health Service Executive andThe Sudan Medical & Specialisation Board (SMSB) | 1 | |||||
| EU Directive 2005/36/EC;EU Directive 2013/55/EU; EU Directive 2018/958/EU | 1 | 1 | 1 | 1 | 1 | 1 |
| Start Year | End Year | |
|---|---|---|
| Memorandum of Agreement Between The Queen’s University of Belfast And Minister for Further and Higher Education, Research, Innovation and Science Ireland And Minister for Health Ireland and Department of Health Northern Ireland | 2024 | 2030 |
| Memorandum of Understanding Between the Health Service Executive and with The College of Physicians and Surgeons Pakistan | 2011 | Ongoing |
| Memorandum of Understanding Between the Health Service Executive andThe Sudan Medical & Specialisation Board (SMSB) | 2017 | Ongoing |
| EU Directive 2005/36/EC;EU Directive 2013/55/EU; EU Directive 2018/958/EU | 2005 | Ongoing |
benefit the health system of my country and partner country(ies)
benefit the health system of my country and partner country(ies)
benefit the health system of my country and partner country(ies)
benefit the health system of my country and partner country(ies)
Government Agreements - 6.1 B
| Start year of implementation: | |
|---|---|
| Memorandum of Agreement Between The Queen’s University of Belfast And Minister for Further and Higher Education, Research, Innovation and Science Ireland And Minister for Health Ireland and Department of Health Northern Ireland | |
| Memorandum of Understanding Between the Health Service Executive and with The College of Physicians and Surgeons Pakistan | 2011 |
| Memorandum of Understanding Between the Health Service Executive andThe Sudan Medical & Specialisation Board (SMSB) | 2017 |
| EU Directive 2005/36/EC;EU Directive 2013/55/EU; EU Directive 2018/958/EU | 2008 |
Agreement: Memorandum of Understanding Between the Health Service Executive and with The College of Physicians and Surgeons Pakistan
| Number of personnel | |
|---|---|
| Doctors | |
| Nurses | |
| Midwives | |
| Dentists | |
| Pharmacists | |
Agreement: Memorandum of Understanding Between the Health Service Executive andThe Sudan Medical & Specialisation Board (SMSB)
| Number of personnel | |
|---|---|
| Doctors | |
| Nurses | |
| Midwives | |
| Dentists | |
| Pharmacists | |
Agreement: EU Directive 2005/36/EC;EU Directive 2013/55/EU; EU Directive 2018/958/EU
| Number of personnel | |
|---|---|
| Doctors | |
| Nurses | |
| Midwives | |
| Dentists | |
| Pharmacists | |
| o Doctors o Nurses o Midwives o Dentists o Pharmacist s o Dietitian o Dispensing Optician o Occupational Therapist o Optometrist o Physiotherapist o Radiation Therapist o Radiographer o Podiatrist o Dental Hygienist o Dental Nurse o Clinical Dental Technician o Orthodontic Therapist o Audiologist o Orthoptist o Psychologist o Advanced Paramedic o Emergency Medical Technician o Paramedic In addition, the Directive relates to professions regulated in other Member States (EEA countries & Switzerland) that are not regulated in Ireland. Those professions regulated in other Member States can be viewed at https://ec.europa.eu/growth/tools-databases/regprof/professions/bycountry | 8,875 medical professionals with Irish qualifications were recognized in another Member State. -16,279 medical profession were recognized in Ireland. Statistics available at https://ec.europa.eu/growth/tools-databases/regprof/statistics/establishment/ranking |
| Upload document(s) | |
|---|---|
| Memorandum of Agreement Between The Queen’s University of Belfast And Minister for Further and Higher Education, Research, Innovation and Science Ireland And Minister for Health Ireland and Department of Health Northern Ireland | |
| Memorandum of Understanding Between the Health Service Executive and with The College of Physicians and Surgeons Pakistan | |
| Memorandum of Understanding Between the Health Service Executive andThe Sudan Medical & Specialisation Board (SMSB) | |
| EU Directive 2005/36/EC;EU Directive 2013/55/EU; EU Directive 2018/958/EU | |
Responsibilities, rights and recruitment practices
Please check all items that apply from the list below:
Please check all items that apply from the list below:
International migration
| Direct (individual) application for education, employment, trade, immigration or entry in country |
Government to government agreements that allow health personnel mobility |
Private recruitment agencies or employer facilitated recruitment |
Private education/ immigration consultancies facilitated mobility |
Other pathways (please specify) | Which pathway is used the most? Please include quantitative data if available. | |
|---|---|---|---|---|---|---|
| Doctors | 1 | 0 | 1 | 0 | Private Recruitment Agencies | |
| Nurses | 1 | 0 | 1 | 1 | Large framework Recruitment | Private Recruitment Agencies |
| Midwives | 1 | 0 | 1 | 1 | Large framework Recruitment | Private Recruitment Agencies |
| Dentists | 1 | 0 | 1 | 0 | EURES | |
| Pharmacists | 1 | 0 | 1 | 1 | ||
| Other occupations | 1 | 0 | 1 | 1 | ||
| Other occupations | 1 | 0 | 1 | 0 | ||
| Other occupations | 1 | 0 | 1 | 0 | ||
| Other occupations | 1 | 0 | 1 | 0 | ||
| Other occupations | 1 | 0 | 1 | 0 |
| Direct (individual) application for education, employment, trade, immigration, or entry in the destination country |
Government to government agreements that allow health personnel mobility |
Private recruitment agencies or employer facilitated recruitment |
Private education/ immigration consultancies facilitated mobility |
Other pathways (please specify) | Which pathway is used the most? Please include quantitative data if available. | |
|---|---|---|---|---|---|---|
| Doctors | 1 | 0 | 1 | 0 | Not currently available. Later in 2024, the MCI will produce a report which will include information on doctors leaving and joining the register | |
| Nurses | 1 | 1 | 1 | 1 | Application for education/employment Application for education/employment | |
| Midwives | 1 | 1 | 1 | 1 | Application for education/employment Application for education/employment | |
| Dentists | 1 | 0 | 1 | 0 | EURES | |
| Pharmacists | 1 | 0 | 1 | 0 | ||
| Other occupations | 1 | 0 | 1 | 0 | ||
| Other occupations | 0 | 0 | 0 | 0 | ||
| Other occupations | 0 | 0 | 0 | 0 | ||
| Other occupations | 0 | 0 | 0 | 0 | ||
| Other occupations | 0 | 0 | 0 | 0 |
Recruitment & migration
Improving the availability and international comparability of data is essential to understanding and addressing the global dynamic of health worker migration. Please consult with your NHWA focal point, if available, to ensure that data reported below is consistent with NHWA reporting*.
(The list of NHWA focal points is available here. Please find the focal point(s) for your country from the list and consult with them.)
For countries reporting through the WHO-Euro/EuroStat/OECD Joint data collection process, please liaise with the JDC focal point.
Inflow and outflow of health personnel
| Doctors | Nurses | Midwives | Dentists | Pharmacists | Remarks | |
|---|---|---|---|---|---|---|
| 2021 | 1707 | 3468 | 27 | 98 | 106 | |
| 2022 | 2192 | 4003 | 47 | 178 | 194 | |
| 2023 | 2266 | 5225 | 84 | 270 | 340 | |
| Data Source (e.g. Regulatory authority, immigration records, work permits, etc.) | Medical Council Data, compiled to fulfil EU Regulation (EU)2022/2294 | NMBI Data, compiled to fulfil EU Regulation (EU)2022/2294 | The Nursing and Midwifery Board of Ireland provided the data directly. | The Dental Council of Ireland provided the below data directly. | The Pharmaceutical Society of Ireland (PSI) provided the below data. Data cut off 23 July 2024. | • Figures in this report many not be directly comparable to other reports from the same data sets due to divergence in methodologies applied by data sources and EU regulatory requirement. |
| Doctors | Nurses | Midwives | Dentists | Pharmacists | Remarks | |
|---|---|---|---|---|---|---|
| 2021 | 191 | |||||
| 2022 | 322 | |||||
| 2023 | ||||||
| Data Source (e.g. letters of good standing, emigration records, government to government agreements etc.) | The Medical Council of Ireland, regulatory body, provided the data below directly. Doctors voluntarily withdrawing from the register. | * Figures in this report are not directly comparable to EU regulation (EU) 2022/2294 due to divergence in methodologies applied by data sources and EU regulatory requirement. *Note on doctors voluntarily withdrawing from the register: Data here refers to doctors who trained in Ireland, who voluntarily withdrew from the register and stated that they intended to ‘practice medicine abroad’. Doctors who did not retain and were removed would not be included and some may have been Irish trained and migrated. * The Nursing and Midwifery Board of Ireland are able to provide data on Certificate of Current Professional Status (CCPS Applications). However, CCPS Request does not directly relate to nurses migrating. * Data on outflows for dentists and pharmacists is not currently available. * Data on emigrating domestically trained health personnel is not available. * For regulated HSCPs, CORU noted that there is some ‘blunt’ data about registrants wishing to be removed from the Register, but what is not stated specifically as a reason to leave by the registrant remains only conjecture. |
Stock of health personnel
For the latest year available, consistent with the National Health Workforce Accounts (NHWA) Indicators 1-07 and 1-08, please provide information on the total stock of health personnel in your country (preferably the active workforce), disaggregated by the place of training (foreign-trained) and the place of birth (foreign-born).
| Medical Doctors (generalist + specialists) | 19328 | 11709 | 7619 | Irish Medical Council - provided data directly. | 2023 | Data provided directly by Medical Council. These figures represent “clinically active”. Figures in this report are not directly comparable to EU regulation (EU) 2022/2294 due to divergence in methodologies applied by data sources and EU regulatory requirement. | |||||
| Nurses | 72543 | 34931 | 37609 | 7713 | 29896 | 39107 | 33436 | NMBI data compiled by Dept of Health to fulfil EU Regulation (EU)2022/2294 | 2023 | Practicing only | |
| Midwives | 4251 | 3298 | 953 | 535 | 418 | 3405 | 846 | NMBI provided data directly | 2023 | Practicing only | |
| Dentists | 3442 | 2145 | 1297 | Register of dentists - Dental Council provided data directly. | 2022 | Data provided directly by Dental Council. Figures in this report are not directly comparable to EU regulation (EU) 2022/2294 due to divergence in methodologies applied by data sources and EU regulatory requirement. | |||||
| Pharmacists | 7578 | 3822 | PSI –The Pharmacy Regulator provided the data directly from the professional register | 2024 | Data provided directly by PSI. Figures in this report are not directly comparable to EU regulation (EU) 2022/2294 due to divergence in methodologies applied by data sources and EU regulatory requirement. |
This information can be provided by one of the following two options:
| Doctors | Nurses | Midwives | Dentists | Pharmacists | |
|---|---|---|---|---|---|
| Total foreign trained personnel | 7619 | 37609 | 953 | 1297 | 3822 |
| Country 1: Top country of training | PAK | IND | GBR | GBR | GBR |
| Country 1: No. of foreign trained health personnel | 1851 | 16851 | 651 | 454 | 2849 |
| Country 2: Top country of training | SDN | GBR | GHA | POL | PRT |
| Country 2: No. of foreign trained health personnel | 1060 | 9917 | 73 | 141 | 181 |
| Country 3: Top country of training | GBR | PHL | ITA | ROU | ESP |
| Country 3: No. of foreign trained health personnel | 709 | 6277 | 60 | 141 | 158 |
| Country 4: Top country of training | ZAF | ZWE | IND | HUN | ITA |
| Country 4: No. of foreign trained health personnel | 513 | 633 | 49 | 106 | 103 |
| Country 5: Top country of training | ROU | NGA | POL | PRT | POL |
| Country 5: No. of foreign trained health personnel | 505 | 558 | 22 | 54 | 97 |
| Country 6: Top country of training | IND | ROU | DEU | ESP | ROU |
| Country 6: No. of foreign trained health personnel | 310 | 495 | 19 | 52 | 81 |
| Country 7: Top country of training | EGY | POL | NGA | LTU | HUN |
| Country 7: No. of foreign trained health personnel | 249 | 464 | 14 | 45 | 53 |
| Country 8: Top country of training | POL | PRT | AUS | IND | ZAF |
| Country 8: No. of foreign trained health personnel | 212 | 234 | 13 | 45 | 30 |
| Country 9: Top country of training | HUN | ESP | GRC | FRA | AUS |
| Country 9: No. of foreign trained health personnel | 206 | 231 | 9 | 29 | 21 |
| Country 10: Top country of training | NGA | USA | ESP | DEU | EGY |
| Country 10: No. of foreign trained health personnel | 125 | 203 | 5 | 26 | 20 |
| Source (e.g. professional register, census data, national survey, other) | Medical Council Register | Nursing and Midwifery Board of Ireland (NMBI) | Nursing and Midwifery Board of Ireland (NMBI) | Dental Council | PSI – The Pharmacy Regulator, professional register of the statutory regulator for pharmacy in Ireland |
| Year of data (Please provide the data of the latest year available) | 2023 | 2023 | 2023 | 2022 | 2024 midpoint |
| Remarks | This data was received directly from the Medical Council. 7,619 doctors qualified outside of Ireland. Primary Qualification Country was available for 7,605 of these doctors. The top 10 countries are outlined above. | These figures refer to practicing only. The data was compiled for this table by the Department of Health, to comply with EU regulation (EU) 2022/2294. Hence, figures in this report many not be not directly comparable to other reports | Figures provided directly from NMBI. | This data was received directly from the regulator (Dental Council). | Note that the UK figures would include a large number of ROI students, but the data only refers to the country where the training was completed |
Technical and financial support
| Country supported | Type of support (please specify) | |
|---|---|---|
| Zambia | Technical assistance to Zambia College of Medicine and Surgery to strengthen capacity for training of medical specialists | |
| Sudan | Collaboration with Sudan Medical Specialization Board on specialist medical training | |
| Country supported | Type of support (please specify) | |
|---|---|---|
| Ethiopia | Technical assistance and training for Ministry of Health on hospital accreditation Training of hospital teams on quality improvement | |
| Mozambique | Training and coaching in quality improvement for Ministry of Health and hospital teams | |
| Tanzania | Technical advice to Ministry of Health and President’s Office for Regional Government and Local Administration for developing national plans and resources to improve quality of care. Benjamin Mkapa Foundation and Amref Health Africa (Irish Mission partners):Through this programme Ireland supports recruitment and deployment of clinicians and nurses to primary health facilities in underserved areas both in Tanzania Mainland and Zanzibar. As part of the agreement with the Ministry of Health, the staff are remunerated for limited period of time and later mainstreamed to the government payroll. Ireland also supports recruitment, training, and deployment of community health workers through this partnership as part of the Government of Tanzania Community Based Health Programme. Ireland provided €1.1 million to this Programme in 2023. Health Basket Fund: The Health Basket Fund (HBF), which is the pooled fund arrangement currently funded by nine donors including Ireland, supports primary healthcare services including Human resources production and capacity development for the mid-level cadres. Ireland contributes € 5 million to the Health Basket Fund annually. The HBF also supported recruitment of over 500 Accountants to support financial management systems at primary healthcare level as part of the Direct Health Facility Financing (DHFF) approach of sending monies directly to local health facilities. These accounts were later on mainstreamed to the government payroll system. | |
| Sudan | In 2023, the HSE provided humanitarian assistance to Sudan, donating €1 million worth of medical equipment and supplies. |
| Country supported | Support Area | Type of support | |
|---|---|---|---|
| East, Central and Southern Africa | Institutional Health Partnership for health workforce development between College of Surgeons of East Central and Southern Africa (COSECSA) and the Royal College of Surgeons in Ireland | Small grant and technical assistance to support postgraduate education and training in Obs and Gynae. | |
| East, Central and Southern Africa | Institutional Health Partnership for health workforce development between College of Obstetricians and Gynaecologists (ECSACOG) and Royal College of Physicians of Ireland | Small grant and technical assistance to support postgraduate education and training in Obs and Gynae. | |
| Tanzania | Institutional partnership for health service strengthening between Irish Blood Transfusion Service (IBTS) and Tanzania National Blood Transfusion Service (NBTS). | Small grant and technical assistance to improve quality of blood transfusion service. |
| Supporting country/entity | Type of support (please specify) | |
|---|---|---|
| European Commission | The Department of Health commenced a project in 2022 supported by the European Union via the Technical Support Instrument, in cooperation with the Directorate-General for Structural Reform Support of the European Commission. The project developed an evidence-based planning tool that has the capacity to produce a variety of workforce projections, under different scenarios with differing types of healthcare policy and reform, and supply side parameters. | |
Constraints, Solutions, and Complementary Comments
| Main constraints | Possible solutions/recommendations | |
|---|---|---|
| Gap between supply and demand of health and social care workers | Strategic partnership agreements; Increase domestic supply | |
| Application by individuals to publicly advertised jobs, and individual applicants seeking to voluntarily relocate to other jurisdictions. | ||
Suggest that some questions could be simplified/ clarified. Some were misinterpreted by stakeholders when responding
Please describe OR Upload (Maximum file size 10 MB)