National Reporting Instrument 2024
Background
[INFOxNRI1]
National Reporting instrument 2024
[BGxINT]
Background
Adopted in 2010 at the 63rd World Health Assembly (WHA Res 63.16), the WHO Global Code of Practice on the International Recruitment of Health Personnel (“the Code”) seeks to strengthen the understanding and ethical management of international health personnel recruitment through improved data, information, and international cooperation.
Article 7 of the Code encourages WHO Member States to exchange information on the international recruitment and migration of health personnel. The WHO Director General is mandated to report to the World Health Assembly every 3 years.
WHO Member States completed the 4th round of national reporting in May 2022. The WHO Director General reported progress on implementation to the 75th World Health Assembly in May 2022 (A75/14). The report on the fourth round highlighted the need to assess implications of health personnel emigration in the context of additional vulnerabilities brought about by the COVID-19 pandemic. For this purpose, the Expert Advisory Group on the relevance and effectiveness of the Code (A 73/9) was reconvened. Following the recommendations of the Expert Advisory Group, the Secretariat has published the WHO health workforce support and safeguards list 2023.
The National Reporting Instrument (NRI) is a country-based, self-assessment tool for information exchange and Code monitoring. The NRI enables WHO to collect and share current evidence and information on the international recruitment and migration of health personnel. The findings from the 5th round of national reporting will be presented to the Executive Board (EB156) in January 2025 in preparation for the 78th World Health Assembly.
The deadline for submitting reports is 31 August 2024.
Article 9 of the Code mandates the WHO Director General to periodically report to the World Health Assembly on the review of the Code’s effectiveness in achieving its stated objectives and suggestions for its improvement. In 2024 a Member-State led expert advisory group will be convened for the third review of the Code’s relevance and effectiveness. The final report of the review will be presented to the 78th World Health Assembly.
For any queries or clarifications on filling in the online questionnaire please contact us at WHOGlobalCode@who.int.
What is the WHO Global Code of Practice?
Disclaimer: The data and information collected through the National Reporting Instrument will be made publicly available via the NRI database (https://www.who.int/teams/health-workforce/migration/practice/reports-database) following the proceedings of the 78th World Health Assembly. The quantitative data will be used to inform the National Health Workforce Accounts data portal (http://www.apps.who.int/nhwaportal/).
Adopted in 2010 at the 63rd World Health Assembly (WHA Res 63.16), the WHO Global Code of Practice on the International Recruitment of Health Personnel (“the Code”) seeks to strengthen the understanding and ethical management of international health personnel recruitment through improved data, information, and international cooperation.
Article 7 of the Code encourages WHO Member States to exchange information on the international recruitment and migration of health personnel. The WHO Director General is mandated to report to the World Health Assembly every 3 years.
WHO Member States completed the 4th round of national reporting in May 2022. The WHO Director General reported progress on implementation to the 75th World Health Assembly in May 2022 (A75/14). The report on the fourth round highlighted the need to assess implications of health personnel emigration in the context of additional vulnerabilities brought about by the COVID-19 pandemic. For this purpose, the Expert Advisory Group on the relevance and effectiveness of the Code (A 73/9) was reconvened. Following the recommendations of the Expert Advisory Group, the Secretariat has published the WHO health workforce support and safeguards list 2023.
The National Reporting Instrument (NRI) is a country-based, self-assessment tool for information exchange and Code monitoring. The NRI enables WHO to collect and share current evidence and information on the international recruitment and migration of health personnel. The findings from the 5th round of national reporting will be presented to the Executive Board (EB156) in January 2025 in preparation for the 78th World Health Assembly.
The deadline for submitting reports is 31 August 2024.
Article 9 of the Code mandates the WHO Director General to periodically report to the World Health Assembly on the review of the Code’s effectiveness in achieving its stated objectives and suggestions for its improvement. In 2024 a Member-State led expert advisory group will be convened for the third review of the Code’s relevance and effectiveness. The final report of the review will be presented to the 78th World Health Assembly.
For any queries or clarifications on filling in the online questionnaire please contact us at WHOGlobalCode@who.int.
What is the WHO Global Code of Practice?
Disclaimer: The data and information collected through the National Reporting Instrument will be made publicly available via the NRI database (https://www.who.int/teams/health-workforce/migration/practice/reports-database) following the proceedings of the 78th World Health Assembly. The quantitative data will be used to inform the National Health Workforce Accounts data portal (http://www.apps.who.int/nhwaportal/).
Disclaimer
[INFOxNRI2]
National Reporting instrument 2024
[disclaim]
Disclaimer
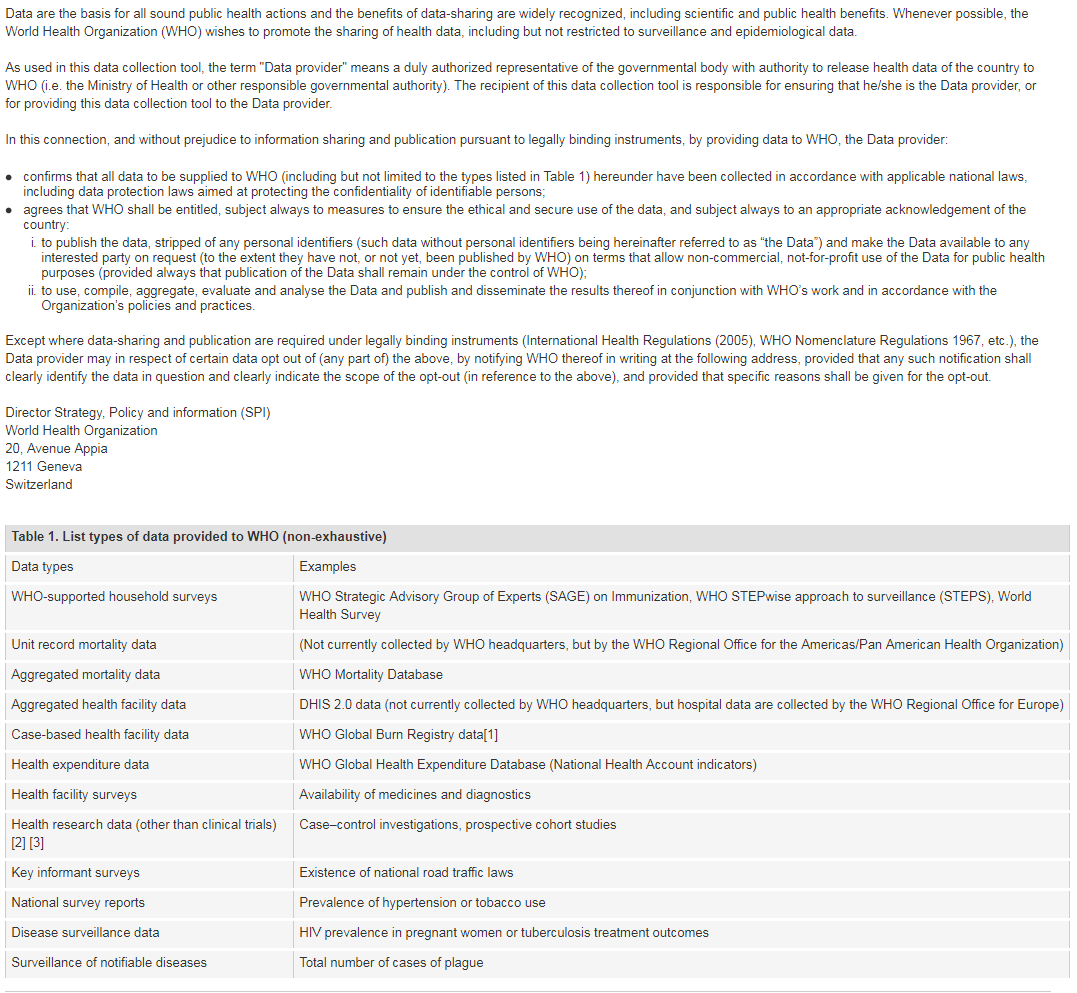
[1] Note: Case-based facility data collection as that in the WHO Global Bum Registry does not require WHO Member State approval.
[2] The world health report 2013: research for universal coverage. Geneva: World Health Organization; 2013 (http://apps.who.int/iris/bitstream/10665/85761/2/9789240690837_eng.pdf)
[3] WHO statement on public disclosure of clinical trial results: Geneva: World Health Organization; 2015 (http://www.who.int/ictrp/results/en/, accessed 21 February 2018).
For more information on WHO Data Policy kindly refer to http://www.who.int/publishing/datapolicy/en/
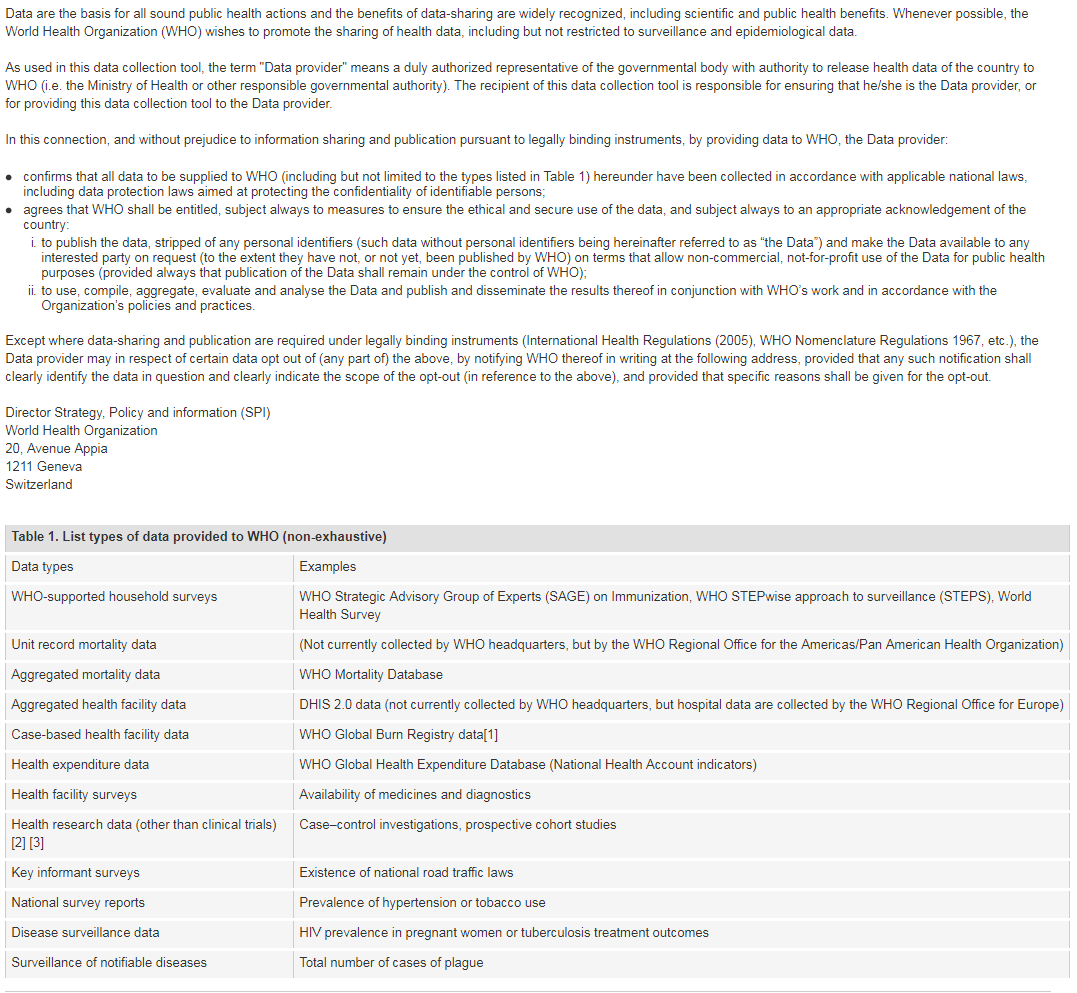
[1] Note: Case-based facility data collection as that in the WHO Global Bum Registry does not require WHO Member State approval.
[2] The world health report 2013: research for universal coverage. Geneva: World Health Organization; 2013 (http://apps.who.int/iris/bitstream/10665/85761/2/9789240690837_eng.pdf)
[3] WHO statement on public disclosure of clinical trial results: Geneva: World Health Organization; 2015 (http://www.who.int/ictrp/results/en/, accessed 21 February 2018).
For more information on WHO Data Policy kindly refer to http://www.who.int/publishing/datapolicy/en/
I have read and understood the WHO policy on the use and sharing of data collected by WHO in Member States outside the context of public health emergencies
Contact Details
[INFOxNRI3]
National Reporting instrument 2024
[CI]
Contact Details
Name of Member State:
Lithuania
Name of designated national authority:
State Accreditation Service for Health Care Activities
Title of designated national authority:
Division of Specialist Activities
Institution of the designated national authority:
State Accreditation Authority for Health Care under the Ministry of Health of the Republic of Lithuania
Email:
riginao@who.int,agne.raukstiene@vaspvt.gov.lt,vaspvt@vaspvt.gov.lt,WHOGlobalCode@who.int
Telephone number :
+370 653 06363
Contemporary issues
[INFOxNRI4]
National Reporting instrument 2024
[NRIxI]
The questions marked * are mandatory. The system will not allow submission until all mandatory questions are answered.
[INFOx1]
Contemporary issues on health personnel migration and mobility
[Q1x1]
In the past 3 years, has the issue of international recruitment of health personnel been a concern for your country?
No, this is not a problem in my country
[Q1x2]
In the past 3 years, has the issue of international reliance on health personnel (international recruitment of health personnel to meet domestic needs) been a concern for your country?
No, this is not a problem in my country
Health Personnel Education
[INFOxNRI5]
National Reporting instrument 2024
[INFOx2]
Health personnel education, employment and health system sustainability
[Q2]
Is your country taking measures to educate, employ and retain a health and care workforce that is appropriate for the specific conditions of your country, including areas of greatest need?
Yes
[Q2x1]
Please check all items that apply from the list below:
2.1 Measures taken to ensure the sustainability of the health and care workforce
2.2 Measures taken to address the geographical mal-distribution and retention of health and care workers*
2.3 Other relevant measures taken to educate, employ and retain a health and care workforce that is appropriate for the specific conditions of your country
[Q2x1x1]
2.1.1 Measures taken to ensure the sustainability of the health and care workforce
Forecasting future health and care workforce requirements to inform planning
The Ministry of Health has developed an action plan for the years 2024-2029 aimed at reducing the uneven distribution of healthcare professionals nationwide and addressing shortages of certain professional qualifications and specializations in the healthcare sector. The action plan outlines the following measures: 1. Monitoring of Healthcare Workforce: Implementation of systems to track and monitor the shortage, training, distribution, and recruitment of healthcare professionals. 2. Improvement of Forecasting and Planning: Enhancements in forecasting and planning for healthcare workforce needs. 3. Empowerment, Recruitment, and Retention: Strategies to empower, attract, and retain healthcare professionals. It is planned to prepare an overview of the current situation of health human resources management in Lithuania, analyze best practices from foreign countries, and provide recommendations for human resources management, demand forecasting, inclusion, retention, improvement, and more. Based on these documents, a long-term health human resources management strategy (up to 2030) would be developed and approved at the national level.
Aligning domestic health and care workforce education with health system needs
Planned Investments in Training and Professional Development. A budget of 30.7 million euros has been allocated for healthcare professionals recruitment measures from the 2021-2027 European Union funds investment program. These funds will be directed towards: • Enhancing Human Resources Management Efficiency: Improving the efficiency of healthcare human resources management. • Financing Study Costs: Covering the costs of healthcare education. • Empowerment, Recruitment, and Retention Models: Developing and implementing models for the empowerment, recruitment, and retention of healthcare professionals within healthcare institutions. • Increasing Prestige and Professional Orientation: Elevating the prestige and professional orientation of the most critically needed professional qualifications and specializations. • Other Related Initiatives: Additional measures to support the overall recruitment and retention strategy.
Improving quality of education and health personnel in alignment with service delivery needs
Ensuring high-quality healthcare services can only be achieved by adequately trained and educated high-level healthcare professionals. To enhance the quality of residency studies and residency bases across the country, the Ministry of Health will allocate funding for the acquisition and improvement of educational competencies of physician residents' mentors – 344,000 euros have been earmarked for this purpose. On July 31, 2024, Order No. V-788 was issued, titled „Order on the approval of the procedure for updating the educational competencies of the resident physician supervisor and acquiring and updating the educational competencies of the resident physician mentor. “ A project funded by the European Union's 2021–2027 investment program is dedicated to physician resident mentors who will work in healthcare institutions outside the largest cities of Lithuania, including regional areas. The project's goal is to provide these mentors with educational skills to ensure a quality learning process and a positive psycho-emotional climate for physician residents in their residency bases. Additionally, it aims to help young doctors integrate more easily and effectively into the healthcare system. Approved professional development programs are designed for healthcare professionals and administrative staff working in personal healthcare institutions. These programs focus on developing both general (management, leadership, communication, emotional literacy, etc.) and specialized competencies. Based on the Long-Term Care Service Provision Model Development Project Plan, which was approved by the Government in December 2021, a plan for the training, retraining, and professional development of long-term care specialists is to be prepared. A legal act aimed at improving the qualifications and working conditions of healthcare professionals is planned to be drafted. This act will regulate the financing mechanism for the professional development of healthcare professionals, introducing a professional qualification development fund for healthcare professionals, financed by the state, institutions, organizations, and personal funds.
Creating employment opportunities aligned with population health needs
Aiming to address the shortage of healthcare professionals in Lithuania's national health system, the Ministry of Health has requested personal healthcare institutions to provide information on their preliminary capabilities to cover the tuition fees of pupils, students, and resident doctors, in accordance with the order of the Minister of Health of the Republic of Lithuania No. V-1080, dated November 7, 2008. Additionally, institutions were asked to provide information on other possible incentive measures for attracting healthcare professionals. The Ministry of Health has compiled lists of incentive measures to present comprehensive information, allowing pupils, students, and resident doctors to find all relevant information in one place and make informed decisions regarding contract agreements with personal healthcare institutions. This list will aid in attracting healthcare professionals with the most needed qualifications to personal healthcare institutions experiencing the greatest shortage of these specialists. These healthcare professionals could contribute to the provision of quality and timely healthcare services, addressing the health needs of the population. Starting from July 1, 2024, a patient transportation service will be launched in Lithuania. Patients who meet the transportation criteria will be able to order the service by calling 1808, from home to the healthcare facility and back. The expansion of this service will bring healthcare services closer to patients and thus help the most vulnerable populations (due to health, poverty, age). The aim of this measure is to ensure that age, level of participation, health status, or other factors do not hinder access to necessary healthcare services.
Managing international recruitment of health personnel
Lithuania adheres to the principles of the World Health Organization (WHO) Global Code of Practice on the International Recruitment of Health Personnel, aiming to ensure ethical and responsible international recruitment of health care professionals. This Code aims to strengthen health systems in developing countries and maintain a balance between the migration of health care professionals and the needs of national health systems. Adherence to Ethical Principles Compliance with the Code: Lithuania is committed to adhering to the WHO Global Code, which sets out ethical principles for the international recruitment of health care professionals, aiming to protect the health systems of developing countries from brain drain. Development of National Strategies Formulating National Policies: The Ministry of Health (SAM) develops national strategies that include measures for the recruitment, training, and retention of health care professionals to ensure that those working in Lithuania meet the country's needs and international standards. International Collaboration Bilateral and Multilateral Agreements: Lithuania collaborates with other countries to ensure fair and responsible recruitment of health care professionals, sharing best practices and information on migration trends. Incentive Programs Incentive Programs: Lithuania implements various incentive measures to retain and attract health care professionals, such as financial support for students, residents, and doctors who commit to working in the country's health care facilities for a specified period. Return Programs Return and Reintegration Programs: Lithuania encourages emigrated health care professionals to return by offering reintegration programs, including professional development, job placements, and financial support. Education and Awareness Information Dissemination: The Ministry of Health and other relevant institutions conduct information campaigns to inform health care professionals about international recruitment rules, opportunities, and responsibilities, as well as the principles of the WHO Code. Challenges and Solutions Shortage of Specialists in Certain Areas Targeted Measures: To address the shortage of specialists, Lithuania implements targeted measures such as financial incentives, professional development programs, and improvements in infrastructure in regional health care facilities. Impact of Migration on the Health System Ensuring Balance: Lithuania strives to maintain a balance between international recruitment of specialists and the needs of the national health system, considering the specifics and priorities of the country's health care sector. Lithuania actively implements measures to ensure responsible international recruitment of health care professionals in accordance with the WHO Global Code of Practice. These measures help strengthen the country's health care system, ensure the sustainability of health care professionals, and contribute to improving public health.
Improving management of health personnel
The Ministry of Health plans to develop and approve professional qualification enhancement programs for healthcare professionals and administrative staff working in personal health care institutions. These programs will focus on both general (management, leadership, communication, emotional intelligence, etc.) and specific competencies. Training sessions are scheduled to commence from 2024 and continue through 2029. An allocation of €1.8 million from the 2021–2027 European Union funds investment program has been designated for this measure. The planned qualification enhancement will focus on primary care, specialized fields (including emergency and urgent medical care, mental health services), long-term care, and pharmacy. It will also include the requalification of emergency medical specialists. To improve the monitoring and planning of healthcare professionals' qualifications, the development of an IT tool—the Healthcare Professionals Competency Platform—is planned.
Specific provisions on health personnel regulation and recruitment during emergencies
Plans are underway for the development and modernization of top-level infectious disease cluster centers and regional infectious disease cluster centers, with an emphasis on improving infectious disease management. Two top-level centers are set to be established for the modernization of emergency medical departments in regional hospitals to ensure effective patient flow management and accessibility and quality of emergency medical services during epidemics/pandemics. A systematic strengthening of the health system's resilience to operate in emergencies is planned, with an allocation of €148 million (excluding VAT) for infrastructure development and equipment acquisition. This initiative aims to ensure regional-level infectious disease treatment capacities during crises (at least 650 beds) and create conditions for conducting research on dangerous and highly dangerous infections, integrating into international scientific programs. The goal is to adapt the emergency medical departments and intensive care units of major national hospitals to effectively provide emergency medical services to a large number of patients simultaneously in the event of high and very high-risk incidents, ensuring safe working conditions for staff working under hazardous conditions. Plans are underway to develop legislation aimed at enhancing the preparedness of healthcare institutions for operating in emergencies. The following actions are planned under the modernization action plan for healthcare institutions' collaboration and infrastructure adaptation for emergencies: Requirements Specification: Establish requirements that healthcare institutions must meet to ensure their preparedness for emergencies. Legal Foundations: Create legal frameworks to support healthcare institutions and their personnel in preparing for and operating during emergencies. Resource Cooperation: Develop legal provisions to facilitate more effective cooperation of resources (material and human). From the 2021-2027 EU funds investment program, it is planned to acquire additional vehicles to meet increased demand due to a higher number of emergency medical service stations and the need to transport patients to specialized centers in acute conditions. This includes updating some vehicles due to wear and tear. On January 18, 2024, an Expert Working Group was established to review healthcare professional education programs and to incorporate competencies necessary for preparedness for emergencies and wartime threats into these programs. The tasks of the Expert Working Group are: To identify the competencies required by healthcare sector professionals to provide rapid and coordinated healthcare services during emergencies or wartime (hereinafter referred to as "competencies"). To establish a strategy for the development of these competencies.
Others
In all cases, the professional qualification of doctors, nurses, dentists, oral care specialists and other regulated professions health care specialists acquired outside the Republic of Lithuania must be recognized in accordance with the Directive 2005/36/EC. Practice shows that the recognition of professional qualification of a medical doctor is recognized by practically all applicants. Problems arise with professional qualification of specialists from third countries, because the duration of studies is often significantly shorter than in Lithuania. During the recognition, the work experience is also assessed. High length of practise sometimes compensates for the shorter duration of studies. Recognition of professional qualifications is only one part of procedure to legally provide personal health care services in Lithuania. Once the professional qualification is recognized, specialist must obtain their license. In order to obtain a license, the conditions for proficiency in the Lithuanian language and permission to temporarily live and work in Lithuania are needed, which often causes problems for individuals.
[Q2x2x1]
Check all that apply for Measures taken to address the geographical mal-distribution and retention of health and care workers
2.2.1 Education
2.2.2 Regulation
2.2.3 Incentives
2.2.4 Support
[Q2x2x1x1]
2.2.1.1 Education Measure
Education institutions based in rural/underserved areas
Educational institutions (universities, colleges, and vocational training schools/centers) are in the major cities of the country.
Student intake from rural/underserved areas and communities
Admissions to educational institutions are carried out according to the general procedure established by the institutions. This procedure allows individuals from rural or underserved areas to apply and be admitted to educational institutions.
Scholarships and subsidies for education
Relevant topics/curricula in education and/or professional development programmes
(Re)orientation of education programmes towards primary health care
Others
[Q2x2x2x1]
2.2.2.1 Regulation Measure
Scholarships and education subsidies with return of service agreements
According to the Order No. V-1080 of November 7, 2008, by the Minister of Health of the Republic of Lithuania, students, trainees, or medical residents can benefit from a legal framework that regulates financial support from municipal administrations or healthcare institutions. This support is available to those studying in non-state-funded places. By entering into study financing agreements, they are required to fulfill contractual obligations by working for a specified number of years in the healthcare institution, thus contributing to the needed healthcare workforce.
Mandatory service agreements with health personnel that are not related to scholarships or education subsidies
Enhanced scope of practice of existing health personnel
Requalification of Emergency Medical Services (EMS) Specialists Starting January 1, 2024, the new regulations for providing Emergency Medical Services (EMS) will come into effect. According to these regulations, EMS drivers will be required to hold a paramedic professional qualification. This change aims to enhance the capabilities of EMS teams, ensuring that all members, including drivers, are equipped with the necessary medical knowledge and skills to effectively respond to emergencies. Pharmacy Specialist Training To better utilize the potential of pharmacists as competent health care specialists, additional training for pharmacy professionals is planned. This training will focus on expanding the range of patient-centered pharmaceutical care services and advanced practice pharmacy roles. Specifically, the following initiatives are planned: 1. Development of Additional Services: By the second half of 2022, a phased implementation of new services provided by pharmacists will begin. This will continue through to 2030, with new regulations defining these services and their delivery conditions. 2. Competency Requirements: Regulations will outline the competencies required for pharmacists, specifying the necessary training hours, procedures, target patient groups, and collaboration with physicians. 3. Enhanced Pharmaceutical Care: The new services will include comprehensive pharmaceutical care and extended practice roles, which will aim to improve patient outcomes through better medication management and health advice. These measures are intended to strengthen the role of pharmacists in the healthcare system, ensuring that they can provide high-quality, patient-focused services and work effectively within the healthcare team.
Task sharing between different professions
Family Doctor Team Model Comprehensive Family Doctor Team: To improve service quality and accessibility, family medicine services are provided by a comprehensive family doctor team. This team includes a family doctor, nurses, midwife, nurse assistant, physiotherapist, lifestyle medicine specialist, and case manager. Competency Distribution: Functions of team members are allocated according to their expanded competencies, thereby more effectively utilizing the specialists' skills. Retraining of Emergency Medical Services Specialists Paramedic Qualification: From January 1, 2024, following the new Emergency Medical Services provision requirements, emergency medical drivers must have a paramedic professional qualification. Retraining Programs: Training and professional development courses are organized to ensure that emergency medical services specialists are adequately prepared for emergencies. Development of Pharmacy Specialists' Competencies Pharmaceutical Care and Advanced Practice Services: To better utilize pharmacists' potential, additional patient-oriented pharmaceutical care and advanced practice pharmacist (pharmacist-healthcare specialist) services are being developed. Regulation and Training: From the second half of 2022 to 2030, it is planned to gradually regulate additional services provided in pharmacies and their conditions, including the enhancement of pharmacists' competencies. Retraining and Professional Development of Specialists Integrated Health Care Services: Continuous training is organized to improve the competencies of health care specialists, providing new knowledge and practical skills for working with innovative and advanced technologies. Retraining for Internal Medicine and Pediatric Doctors: There are plans to allow internal medicine and pediatric doctors to additionally obtain family doctor qualifications. Practical Implementation Examples Competency Platform Health Care Specialist Competency Platform: An IT tool is planned to be created to monitor and plan the professional development and practical skills acquisition processes of health care specialists. Regional Initiatives Strengthening Regional Health Care Centers: Projects are being carried out in regional health care centers to strengthen the composition and competencies of specialist teams, thereby ensuring better service accessibility.
Provisions for pathways to enter new or specialised practice after rural service
The Ministry of Health has initiated changes to the Regulations for the Implementation and Supervision of Medical Residency and Dental Residency Programs, as approved by the Government's decree. The changes, effective from January 1, 2023, include extending the duration of certain residency programs and introducing a minimum requirement for professional practice. Specifically, by 2027, at least 35% of medical residents' professional practice must be completed outside university hospitals. To qualify as a residency base, healthcare institutions now only need to have a medical resident mentor (a new role) responsible for overseeing the acquisition of practical skills by medical residents, replacing the previous requirement for a medical resident supervisor. Funds from the initiative will be used to train doctors who wish to become medical resident mentors. Additionally, the Ministry of Health is implementing an EU-funded project titled "Recruiting Specialists to Reduce Health Disparities" (Project No. 08.4.2-ESFA-V-617), with a budget of €668,800. This project aims to fund residency training for doctors (at least 34 individuals) who commit to working for a minimum of 2 years in healthcare facilities in specific districts, as stipulated in their agreements.
Others
[Q2x2x3x1]
2.2.3.1 Incentives Measure
Additional financial reimbursement
Additional Salary Supplements: Health professionals working in regions or specialties with significant shortages may receive additional salary supplements. These supplements aim to make positions in underserved or high-need areas more attractive. Retention Bonuses: Financial bonuses are offered to healthcare workers who commit to staying in their positions for an extended period, particularly in areas with high demand or difficult working conditions. Financial Support for Education and Training Study Funding: Financial support is provided to cover the costs of education for students pursuing degrees in health-related fields. This can include scholarships or loans that are partially forgiven if the recipient works in designated underserved areas. Training and Certification Costs: Funds are allocated to cover the costs of professional development and certification for existing health care professionals. This includes costs associated with additional qualifications, specialized training, and continuing education. Support for Recruitment and Retention Relocation Assistance: Financial aid is provided to healthcare professionals who relocate to work in high-need areas. This can include relocation expenses, housing allowances, and other support to ease the transition. Employment Grants: Grants or subsidies are offered to health care institutions to support the hiring of additional staff. These funds can help offset the costs associated with expanding services or increasing staff numbers. Incentives for Mentorship and Supervision Mentorship Stipends: Financial incentives are offered to experienced professionals who take on mentorship roles, particularly in training new specialists or supervising their work. This aims to encourage experienced professionals to share their knowledge and support the development of new talent. Supervision Allowances: Additional funding is provided to institutions that facilitate supervision and support for new or less experienced health care professionals. Bonuses for Extra Duties and Responsibilities Performance-Based Bonuses: Health professionals who take on additional duties or responsibilities beyond their standard roles may receive performance-based bonuses. This includes taking on extra shifts, working in challenging conditions, or providing additional services. Specialty Bonuses: Additional financial incentives are given to professionals who acquire specialized skills or work in high-demand specialties, such as emergency medicine, psychiatry, or geriatrics. Implementation and Monitoring Evaluation and Adjustments: The effectiveness of these financial measures is regularly evaluated to ensure they meet their goals of addressing shortages and improving workforce retention. Adjustments are made based on feedback from health professionals and performance data. Transparency and Communication: Clear communication about available financial support and eligibility criteria is essential to ensure that health professionals are aware of the incentives and can access them effectively.
Education opportunities
To ensure the occupancy of state-funded study places and to enhance the prestige of certain professional qualifications, as well as to encourage professional orientation and shift public perceptions about specific healthcare professions, the following communication activities are planned: 1. Sharing Professional Experience: Healthcare professionals (preferably from the same cities) will visit schools and high schools to share their professional experiences and career paths. 2. Encouragement Events: Events, practical assignments, and tours of healthcare institutions will be organized to motivate students to choose healthcare professions, providing them with a clearer understanding of the benefits and challenges of these careers. 3. Information Dissemination for Medical Students: Dissemination of information among medical students in integrated studies, guiding them to choose the most needed qualifications after six years of study, such as family medicine, emergency medicine, geriatrics, and psychiatry. 4. Information Dissemination for Nursing Students: Information dissemination and incentives will be targeted at general practice nursing students to better inform them about their career options and opportunities in the healthcare sector. These activities aim to shift societal attitudes towards healthcare professions and encourage young people to pursue careers in this field.
Opportunities for career advancement or professional growth
To enhance the competencies of healthcare professionals and other specialists in the healthcare field and ensure continuous professional development, the goal is to provide new knowledge and improve practical skills. This includes integrating advanced healthcare services and working with innovative, cutting-edge technologies. From the 2014-2020 EU funding period and the 2014-2021 European Economic Area Financial Mechanism "Health" program, various projects were implemented to enhance specialists' qualifications. However, due to the ongoing need for continuous improvement to enhance service quality, qualifications development and retraining activities will continue into the 2022-2030 period. Experiences from pandemic management encourage the exploration of solutions to strengthen primary healthcare, expand telemedicine and mobile service options (such as remote consultations, patient monitoring, home visits by family doctors, emotional support, health maintenance advice, etc.). Advances in health technology and the precision of diagnostic and treatment methods are altering the roles of various professions in the treatment process and presenting new challenges for ensuring the safety and quality of health services. This involves planning, evaluating, maintaining, and improving the competencies of healthcare professionals to meet medical standards and creating favorable conditions for implementing innovative healthcare service delivery models. In restructuring the network of healthcare institutions, the aim is to ensure that primary care services within the scope of family medicine are provided exclusively by a fully-fledged family medicine team. This team would include a family doctor, nurses, a midwife, a nursing assistant, a physiotherapist, a lifestyle medicine specialist, and a case manager. The functions of team members should be allocated based on their developed competencies to enhance service quality and accessibility through more effective use of specialist skills. For a fully integrated family medicine team, it is essential to ensure not only a complete composition of required specialists but also the redistribution of their responsibilities, ongoing qualification improvement/retraining (e.g., internal medicine and pediatric specialists could acquire additional qualifications in family medicine), adaptation of existing service delivery methodologies, algorithms, and recommendations, as well as the development and implementation of new ones.
Professional recognition
Social recognition
Public Visibility: The activities of healthcare professionals are often highlighted through media, social networks, and other communication channels. This helps the public learn about their achievements and contributions to the healthcare system. Awards and Recognition Ceremonies: Awards ceremonies are held to honor healthcare professionals who have achieved significant results or contributed to important projects. These awards may be given by the state, municipalities, or professional associations. Patient Feedback: Patient reviews and gratitude letters are also considered important aspects of social recognition. Many healthcare professionals receive positive feedback from patients who value their work and commitment. Professional Organization Recognition: Professional organizations and associations evaluate and acknowledge the contributions and achievements of specialists, granting them certificates, titles, or other recognition markers. Educational and Public Awareness Activities Profession Promotion in Schools and Universities: Events, seminars, and practical tasks are organized in schools and universities where professionals share their experiences with young people. This helps improve the image of the profession and encourages youth to choose a career in healthcare. Public Awareness Campaigns: Organizations and institutions run campaigns to increase public understanding of the work and importance of healthcare professionals. This may include advertising campaigns, social media posts, informational posters, and more. Documentation of Professional Achievements Professional Achievements Documentation: Healthcare professionals can be recognized for their achievements, such as scientific research, innovations, or exceptional services. These achievements can be published in scientific journals, healthcare magazines, or other sources. Social Responsibility Projects: Involvement in social responsibility projects, such as free health screenings, educational programs, or assistance to socially vulnerable groups, also contributes to social recognition. Participation in International Projects International Projects and Collaboration: Participation in international healthcare projects and collaboration with foreign professionals provides opportunities for international recognition and experience, which can enhance social recognition at the national level. Career and Professional Development Career Opportunities: Various career development and professional growth opportunities are provided, including leadership positions, teaching, and mentoring roles, which help professionals gain recognition for their contributions and experience in the healthcare system.
Opportunity for pathways to permanent residency and/or citizenship for international health personnel
Others
[Q2x2x4x1]
2.2.4.1 Support Measure
Decent and safe working conditions
Health and Safety Regulations Occupational Health and Safety Standards: Lithuania adheres to strict occupational health and safety regulations that apply to all workplaces, including healthcare facilities. These regulations ensure that healthcare professionals work in environments that minimize risks and protect their health. Regular Safety Inspections: Healthcare facilities undergo regular safety inspections to ensure compliance with health and safety standards. This includes checking for proper sanitation, ergonomic workplace design, and adequate safety equipment. Workplace Safety Training Mandatory Training Programs: Healthcare professionals are required to undergo regular training in workplace safety, including emergency procedures, infection control, and proper use of personal protective equipment (PPE). Continuing Education: Ongoing education programs are provided to keep healthcare workers informed about the latest safety protocols, technological advancements, and best practices. Supportive Work Environment Ergonomic Workspaces: Facilities are designed to be ergonomic, reducing physical strain and preventing injuries. This includes adjustable furniture, proper lighting, and equipment designed to minimize physical effort. Mental Health Support: Recognizing the high stress associated with healthcare professions, mental health support and counseling services are available to help professionals manage stress and prevent burnout. Infection Control Measures Infection Prevention Protocols: Healthcare settings are equipped with rigorous infection control protocols to protect staff from exposure to harmful pathogens. This includes regular disinfection of surfaces, proper waste management, and protocols for handling infectious materials. Vaccination Programs: Vaccination programs are in place to protect healthcare professionals from infectious diseases. These programs are regularly updated based on current health threats. Fair Compensation and Benefits Competitive Salaries: Efforts are made to ensure that salaries for healthcare professionals are competitive and reflect the high level of responsibility and expertise required. Additional Benefits: Healthcare professionals receive additional benefits such as health insurance, paid leave, and retirement plans, contributing to their overall job satisfaction and security. Work-Life Balance Flexible Scheduling: Initiatives to improve work-life balance include flexible scheduling options and support for part-time work or job-sharing arrangements. Leave Policies: Generous leave policies, including sick leave, parental leave, and vacation time, are in place to help professionals manage their personal and family responsibilities. Emergency Preparedness Preparedness Plans: Healthcare facilities have emergency preparedness plans in place for dealing with crises such as natural disasters, pandemics, or mass casualty events. These plans are regularly reviewed and updated. Crisis Training: Regular crisis management training ensures that healthcare professionals are prepared to handle emergencies effectively and safely. Legal Protections Legal Framework: Lithuanian labor laws provide protections for healthcare professionals, including regulations on working hours, breaks, and conditions of employment. Reporting Mechanisms: There are established mechanisms for reporting unsafe working conditions or occupational hazards, ensuring that concerns are addressed promptly and effectively.
Decent and safe living conditions
Distance learning/e-learning opportunities
Others
[Q3x1]
Are there specific policies and/or laws that guide international recruitment, migration and integration of foreign-trained health personnel in your country?
No
[Q3x2]
Are there any policies and/or provision for international telehealth services in your country through health personnel based abroad?
No
[Q3x3]
Has your country established a database or compilation of laws and regulations related to international health personnel recruitment and migration and, as appropriate, information related to their implementation?
No
[Q4]
Recognizing the role of other government entities, does the Ministry of Health have mechanisms (e.g. policies, processes, unit) to monitor and coordinate across sectors on issues related to the international recruitment and migration of health personnel?
No
[Q5]
Please describe the steps taken by your country to implement the following Code recommendations.
Check all items that apply from the list below:
Check all items that apply from the list below:
5.1 Measures have been taken or are being considered to introduce changes to laws or policies on health personnel consistent with the recommendations of the Code.
On July 31, 2024, Order No. V-788 was issued, titled “Order on the approval of the procedure for updating the educational competencies of the resident physician supervisor and acquiring and updating the educational competencies of the resident physician mentor.”
5.2 Actions have been taken to communicate and share information across
sectors on the international recruitment and migration of health personnel, as well as to publicize the Code, among relevant ministries, departments and agencies,
nationally and/or sub-nationally.
sectors on the international recruitment and migration of health personnel, as well as to publicize the Code, among relevant ministries, departments and agencies,
nationally and/or sub-nationally.
On July 5, 2024, at the national and / or regional level, a letter titled “Request to provide information and conduct active communication“ was sent to healthcare institutions. The purpose was to gather information on all agreements established and terminated by healthcare institutions and/or municipalities regarding the employment of specialists under contractual obligations. Additionally, the letter requested information on the incentive measures implemented by healthcare institutions to attract health specialists, as well as details regarding vacant positions for healthcare specialists.
5.3 Measures have been taken to consult stakeholders in decision-making
processes and/or involve them in activities related to the international recruitment of health personnel.
processes and/or involve them in activities related to the international recruitment of health personnel.
See the previous information provided in section 5.2
5.4 Records are maintained on all private recruitment agencies for health
personnel authorized by competent authorities to operate within their jurisdiction.
personnel authorized by competent authorities to operate within their jurisdiction.
5.5 Good practices, as called for by the Code, are encouraged and promoted among private recruitment agencies.
5.5a Promotion of the Code among private recruitment agencies.
5.5b Domestic legislation or policy requiring ethical practice of private recruitment agencies, as consistent with the principles and articles of the Code.
5.5c Public or private certification of ethical practice for private recruitment agencies.
5.5d Others
5.6 None of the above
Government Agreements
[INFOxNRI6]
National Reporting instrument 2024
[INFOx3]
Government-to-Government agreements on migration or mobility of health personnel
[Q6]
Has your country or sub-national governments entered into any bilateral, multilateral, or regional agreements and/or arrangements with respect to the international recruitment and/or mobility of health personnel?
No
Responsibilities, rights and recruitment practices
[INFOxNRI9]
National Reporting instrument 2024
[INFOx4]
Responsibilities, rights and recruitment practices
[Q7]
If your country employs/hosts international health personnel to work in the health and care sectors, which legal safeguards and/or other mechanisms are in place for migrant health personnel and to ensure that enjoy the same legal rights and responsibilities as the domestically trained health workforce?
Please check all items that apply from the list below:
Please check all items that apply from the list below:
Migrant health personnel are recruited using mechanisms that allow them to assess the benefits and risk associated with employment positions and to make timely and informed decisions on the employment.
Migrant health personnel are hired, promoted and remunerated based on objective criteria such as levels of qualification, years of experience and degrees of professional responsibility on the same basis as the domestically trained health workforce.
The same conditions and requirements are applied as for Lithuanian health care specialists
Migrant health personnel enjoy the same opportunities as the domestically trained health workforce to strengthen their professional education, qualifications and career progression.
The same conditions and requirements are applied as for Lithuanian health care specialists
Institutional arrangements are in place to ensure safe migration/ mobility and integration of migrant health personnel.
Measures have been taken to promote circular migration of international health personnel
Other measures (including legal and administrative) for fair recruitment and employment practices of foreign-trained and/or immigrant health personnel (please provide details)
No measures in place
Not applicable – does not host/employ foreign health personnel
[Q8]
If health personnel from your country are working abroad in the health and care sectors, please provide information on measures that have been taken or are planned in your country to ensure their fair recruitment and employment; safe migration; return; and diaspora utilization in your country, as well as difficulties encountered.
Please check all items that apply from the list below:
Please check all items that apply from the list below:
Arrangements for fair recruitment
Arrangements for decent employment contracts and working conditions in destination countries
Arrangements for safe mobility
Arrangements for return and reintegration to the health labour market in your country
Arrangements for diaspora engagement to support your country health system
Other
No measures in place
The same conditions and requirements are applied as for Lithuanian health care specialists
Not applicable – health personnel from my country are not working abroad
International migration
[INFOxNRI10]
National Reporting instrument 2024
[INFOx5]
International migration and mobility pathways for health personnel
[Q9x1]
9.1 If your country hosts international health personnel to work in the health and care sector, how do they come to your country? (check all that apply)
| Direct (individual) application for education, employment, trade, immigration or entry in country |
Government to government agreements that allow health personnel mobility |
Private recruitment agencies or employer facilitated recruitment |
Private education/ immigration consultancies facilitated mobility |
Other pathways (please specify) | Which pathway is used the most? Please include quantitative data if available. | |
|---|---|---|---|---|---|---|
| Doctors | 1 | 0 | 1 | 0 | ||
| Nurses | 1 | 0 | 1 | 0 | ||
| Midwives | 1 | 0 | 1 | 0 | ||
| Dentists | 1 | 0 | 1 | 0 | ||
| Pharmacists | 1 | 0 | 1 | 0 | ||
| Other occupations | 0 | 0 | 0 | 0 | ||
| Other occupations | 0 | 0 | 0 | 0 | ||
| Other occupations | 0 | 0 | 0 | 0 | ||
| Other occupations | 0 | 0 | 0 | 0 | ||
| Other occupations | 0 | 0 | 0 | 0 |
[Q9x1oth]
[Q9x2]
9.2 If health personnel from your country work/study abroad, how do they leave your country?
(check all that apply)
| Direct (individual) application for education, employment, trade, immigration, or entry in the destination country |
Government to government agreements that allow health personnel mobility |
Private recruitment agencies or employer facilitated recruitment |
Private education/ immigration consultancies facilitated mobility |
Other pathways (please specify) | Which pathway is used the most? Please include quantitative data if available. | |
|---|---|---|---|---|---|---|
| Doctors | 1 | 0 | 1 | 0 | ||
| Nurses | 1 | 0 | 1 | 0 | ||
| Midwives | 1 | 0 | 1 | 0 | ||
| Dentists | 1 | 0 | 1 | 0 | ||
| Pharmacists | 1 | 0 | 1 | 0 | ||
| Other occupations | 0 | 0 | 0 | 0 | ||
| Other occupations | 0 | 0 | 0 | 0 | ||
| Other occupations | 0 | 0 | 0 | 0 | ||
| Other occupations | 0 | 0 | 0 | 0 | ||
| Other occupations | 0 | 0 | 0 | 0 |
[Q9x2oth]
Recruitment & migration
[INFOxNRI11]
National Reporting instrument 2024
[INFOx6]
Data on international health personnel recruitment & migration
Improving the availability and international comparability of data is essential to understanding and addressing the global dynamic of health worker migration. Please consult with your NHWA focal point, if available, to ensure that data reported below is consistent with NHWA reporting*.
(The list of NHWA focal points is available here. Please find the focal point(s) for your country from the list and consult with them.)
For countries reporting through the WHO-Euro/EuroStat/OECD Joint data collection process, please liaise with the JDC focal point.
[Q10]
Does your country have any mechanism(s) or entity(ies) to maintain statistical records of foreign-born and foreign-trained health personnel?
Yes
[Q10x1]
Where are the records maintained? (check all that apply)
Employment records or work permits
Ministry of health personnel database
Registry of health personnel authorized to practice
Other
[Q10x2]
Does the record include gender-disaggregated data on the foreign-born and/or foreign-trained health personnel?
Yes
Inflow and outflow of health personnel
[INFOxNRI12]
National Reporting instrument 2024
[INFOx7]
Inflow and outflow of health personnel
[Q11]
Do you have a mechanism to monitor the inflow and outflow of health personnel to/from your country? (check all that apply)
Inflow
Outflow
No
[Q11xI]
If yes for inflow:
[Q11x1]
How many foreign-trained or foreign-born health personnel were newly active (temporarily and/or permanently) in your country in the past three years (inflow)?
| Doctors | Nurses | Midwives | Dentists | Pharmacists | Remarks | |
|---|---|---|---|---|---|---|
| 2021 | 42 | 4 | 3 | 9 | 0 | |
| 2022 | 130 | 51 | 0 | 45 | 3 | |
| 2023 | 92 | 58 | 2 | 32 | 16 | |
| Data Source (e.g. Regulatory authority, immigration records, work permits, etc.) | Register of health care and pharmacy practice licenses | Register of health care and pharmacy practice licenses | Register of health care and pharmacy practice licenses and Compulsory Health Insurance Fund Information System, licenced specialists | Register of health care and pharmacy practice licenses and Compulsory Health Insurance Fund Information System, licenced specialists | Register of health care and pharmacy practice licenses |
[Q11x3]
If you have any document with information on health worker inflows and outflows for your country, please upload
Stock of health personnel
[INFOxNRI13]
National Reporting instrument 2024
[INFOx8]
Stock of health personnel
[Q12x1]
Consolidated stock on health personnel, disaggregated by place of training and birth
For the latest year available, consistent with the National Health Workforce Accounts (NHWA) Indicators 1-07 and 1-08, please provide information on the total stock of health personnel in your country (preferably the active workforce), disaggregated by the place of training (foreign-trained) and the place of birth (foreign-born).
For the latest year available, consistent with the National Health Workforce Accounts (NHWA) Indicators 1-07 and 1-08, please provide information on the total stock of health personnel in your country (preferably the active workforce), disaggregated by the place of training (foreign-trained) and the place of birth (foreign-born).
[Q12x1a]
Please provide data on the stock of active health personnel in your country by one of the following ways:
Fill in the table below
[Q12x1x1]
| Medical Doctors (generalist + specialists) | 17421 | 17101 | 186 | Hygiene institute and Register of health care and pharmacy practice licenses | 2023 | ||||||
| Nurses | 26769 | 26492 | 216 | Hygiene institute and Register of health care and pharmacy practice licenses | 2023 | ||||||
| Midwives | 1089 | 1084 | 5 | Hygiene institute and Register of health care and pharmacy practice licenses | 2023 | ||||||
| Dentists | 4806 | Hygiene institute and Register of health care and pharmacy practice licenses | 2023 | ||||||||
| Pharmacists | 3536 | 3515 | 19 | Hygiene institute and Register of health care and pharmacy practice licenses | 2023 |
[Q12x1x1x]
If you have any document with information on stock of active health personnel for your country, their distribution by place of training and place of birth, please upload
[Q12x2]
Please provide data on the top 10 countries of training for foreign-trained health personnel in your country.
This information can be provided by one of the following two options:
This information can be provided by one of the following two options:
Fill in the table below
[Q12x2x1]
| Doctors | Nurses | Midwives | Dentists | Pharmacists | |
|---|---|---|---|---|---|
| Total foreign trained personnel | 186 | 216 | 5 | 19 | |
| Country 1: Top country of training | UKR | UKR | UKR | UKR | |
| Country 1: No. of foreign trained health personnel | 103 | 103 | 2 | 16 | |
| Country 2: Top country of training | RUS | RUS | RUS | RUS | |
| Country 2: No. of foreign trained health personnel | 25 | 35 | 2 | 3 | |
| Country 3: Top country of training | BLR | BLR | BLR | ||
| Country 3: No. of foreign trained health personnel | 36 | 38 | 1 | ||
| Country 4: Top country of training | EST | POL | |||
| Country 4: No. of foreign trained health personnel | 7 | 15 | |||
| Country 5: Top country of training | KAZ | LVA | |||
| Country 5: No. of foreign trained health personnel | 4 | 17 | |||
| Country 6: Top country of training | AZE | ||||
| Country 6: No. of foreign trained health personnel | 2 | ||||
| Country 7: Top country of training | |||||
| Country 7: No. of foreign trained health personnel | |||||
| Country 8: Top country of training | |||||
| Country 8: No. of foreign trained health personnel | |||||
| Country 9: Top country of training | |||||
| Country 9: No. of foreign trained health personnel | |||||
| Country 10: Top country of training | |||||
| Country 10: No. of foreign trained health personnel | |||||
| Source (e.g. professional register, census data, national survey, other) | |||||
| Year of data (Please provide the data of the latest year available) | 2023 | 2023 | 2023 | 2023 | |
| Remarks |
[Q12x2x1x]
If you have any document with information on the distribution of foreign-trained health personnel for your country by their country of training, please upload
Technical and financial support
[INFOxNRI14]
National Reporting instrument 2024
[INFOx9]
Technical and financial support
[Q13]
Has your country provided technical or financial assistance to any source countries or countries in the WHO health workforce support and safeguards list 2023, or other low- and middle-income countries on health workforce development, health system strengthening, or for implementing other recommendations of the Code (e.g., strengthening data, information and research on health workforce for translation to policies and planning, etc.)
No
[Q14]
Has your country received technical or financial assistance from any WHO Member State or other stakeholders (e.g., development partners, other agencies) for health workforce development, health system strengthening, or for implementing other recommendations of the Code (e.g., strengthening data, information and research on health workforce for translation to policies and planning, etc.)?
Yes
[Q14x]
Please provide additional information below (check all that apply):
Support for health workforce development (planning, education, employment, retention)
Support for other elements for health system strengthening (service delivery; health information systems; health financing; medical products and technology; and health leadership and governance)
Other areas of support:
[Q14x1]
Please specify support for health workforce development (planning, education, employment, retention)
| Supporting country/entity | Type of support (please specify) | |
|---|---|---|
| Europe Union | Lithuania has accessed significant financial support from European Union (EU) structural funds for health system strengthening. These funds have been used to improve healthcare infrastructure, enhance the skills of the health workforce, and implement various health reforms aimed at increasing efficiency and quality in the healthcare system. | |
| Nordic Countries | Partnerships with Nordic Countries: Lithuania has engaged in partnerships with Nordic countries, particularly through the Nordic Council of Ministers, for collaborative projects focused on health system strengthening and workforce development. These partnerships often involve sharing best practices, training, and capacity building. | |
| Norway, Sweden and Germany | Lithuania has also received support from various development partners, including bilateral assistance from countries like Norway, Sweden, and Germany. These countries have provided both technical expertise and funding for projects related to health workforce development, including training programs, exchange of knowledge, and implementation of health system reforms. | |
[Q14x2]
Please specify support for other elements of health system strengthening (service delivery; health information systems; health financing; medical products and technology; and health leadership and governance)
| Supporting country/entity: | Type of support (please specify) | |
|---|---|---|
| Europe Union | Technical support was received in the form of COVID-19 tests, vaccines, and other technical tools to facilitate the work of healthcare professionals during the pandemic. | |
Constraints, Solutions, and Complementary Comments
[INFOxNRI15]
National Reporting instrument 2024
[INFOx10]
Constraints, Solutions, and Complementary Comments
[Q15]
Please list in priority order, the three main constraints to the ethical management of international migration in your country and propose possible solutions:
| Main constraints | Possible solutions/recommendations | |
|---|---|---|
| Social Integration and Public Perception | Public Awareness Campaigns: Implement targeted campaigns to promote the benefits of migration and multiculturalism, emphasizing success stories and contributions of migrants. | |
| Policy and Legal Framework | Policy Reform: Update and harmonize migration laws to align with international human rights standards, ensuring that they are flexible enough to respond to evolving migration patterns. International Cooperation: Strengthen bilateral and multilateral agreements with source countries to manage migration flows more effectively and humanely. | |
| Economic Integration | Recognition of Qualifications: Simplify and streamline the process for recognizing foreign qualifications and work experience, allowing migrants to work in their trained professions. Entrepreneurship Support: Provide resources, mentoring, and financial support for migrants interested in starting their own businesses, which can create jobs and stimulate the local economy. |
[Q16]
What support do you require to strengthen implementation of the Code?
Support to strengthen data and information on health personnel
1. Enhanced Data Collection Systems Develop Comprehensive Databases: Create or improve national health personnel databases that capture detailed and up-to-date information on the workforce, including demographics, qualifications, and employment status. Implement Standardized Data Collection Tools: Use standardized tools and methods for collecting data across different regions and institutions to ensure consistency and comparability. 2. Data Analysis and Reporting Build Analytical Capacity: Train staff in data analysis techniques to interpret health workforce data effectively, identify trends, and make data-dr,iven decisions. Generate Regular Reports: Produce and disseminate regular reports on health personnel statistics, including workforce distribution, shortages, and migration patterns. 3. Integration with Health Information Systems Link Data Systems: Integrate health personnel data with broader health information systems to provide a comprehensive view of health service delivery and needs. Ensure Interoperability: Ensure that data systems are interoperable with international databases and frameworks to facilitate comparison and coordination. 4. Data Quality and Validation Implement Quality Assurance Measures: Establish procedures for data validation and quality assurance to ensure the accuracy and reliability of health personnel data. Conduct Regular Audits: Perform regular audits of data collection processes and systems to identify and address issues affecting data quality. 5. Capacity Building and Training Train Data Collectors and Analysts: Provide training for personnel involved in data collection and analysis to enhance their skills and understanding of best practices. Develop Data Management Skills: Offer courses and workshops on data management, including the use of advanced data analysis tools and techniques. 6. Access to Technology and Tools Provide IT Infrastructure: Ensure that health institutions have access to the necessary IT infrastructure and software for effective data collection and management. Support Innovative Solutions: Encourage the adoption of innovative technologies such as mobile data collection apps and cloud-based systems to streamline data processes. 7. Collaboration and Partnerships Engage with International Organizations: Collaborate with international organizations and agencies to access best practices, benchmarks, and support for data initiatives. Foster Interinstitutional Cooperation: Promote cooperation between different institutions and agencies involved in health workforce data collection and management. 8. Public Awareness and Transparency Share Data Publicly: Increase transparency by making health workforce data publicly available, where appropriate, to support accountability and informed decision-making. Promote Data Literacy: Raise awareness about the importance of data and its role in improving health systems, and encourage stakeholders to use data in planning and policy development. 9. Policy and Regulatory Support Establish Data Governance Policies: Develop and implement policies for data governance, including data privacy, security, and ethical considerations. Create Data Standards: Define and enforce standards for data collection, reporting, and analysis to ensure consistency and quality.
Support for policy dialogue and development
Support for the development of bilateral/multi-lateral agreements
Others
No support required
[Q17]
Considering that the Code is a dynamic document that should be updated as required, please provide reflections from your country on the past 14 years since the resolution on the Code.
[Q17x1]
Please comment on if/how the Code has been useful to your country.
Evolving Policy and Regulatory Framework
Adoption and Integration:
Since the adoption of the Code in 2010, Lithuania has progressively integrated its principles into national policies. This has involved aligning local regulations with the Code’s recommendations to ensure ethical recruitment practices and prevent the migration of health personnel from low-resource settings.
Regulatory Updates:
The legal framework has been periodically updated to better align with the Code’s recommendations. This includes regulations governing international recruitment, professional standards, and measures to avoid practices that could negatively impact developing countries.
Enhancing Domestic Workforce Capacity
Training and Education:
Efforts have been made to improve the education and training of domestic health personnel to reduce dependency on international recruitment. This includes expanding medical education opportunities and increasing the capacity of training institutions.
Professional Development:
Continuous professional development programs have been established to ensure that health personnel are equipped with the latest skills and knowledge, thus enhancing the quality of care and reducing the need for international recruitment.
Ethical Recruitment Practices
Monitoring and Compliance:
The country has implemented mechanisms to monitor compliance with ethical recruitment practices. This involves ensuring that recruitment agencies and employers adhere to standards that prevent the exploitation of health personnel from developing countries.
International Collaboration:
Lithuania has engaged in international cooperation to share best practices and collaborate on initiatives that support the Code’s objectives. This includes working with global health organizations and participating in international forums.
Addressing Domestic Needs and Retention
Incentives and Retention Strategies:
To address shortages and retain domestic health personnel, various incentives have been introduced, such as financial benefits, career development opportunities, and improved working conditions.
Public Awareness and Recognition:
Efforts to enhance the social recognition of health professions and promote career paths in healthcare have been undertaken. This includes public campaigns to highlight the value of health workers and their contributions to society.
Evaluating Impact and Adjusting Strategies
Regular Review and Feedback:
The impact of the Code’s implementation has been regularly reviewed through feedback mechanisms, including surveys and evaluations of recruitment practices and workforce conditions. This has helped to identify areas for improvement and adjust strategies accordingly.
Adaptation to Emerging Challenges:
The dynamic nature of the Code has necessitated periodic adjustments to national policies and strategies to address emerging challenges and opportunities in the global health workforce landscape.
[Q17x2]
Do any articles of the Code need to be updated?
No
[Q17x3]
Does the process of reporting on Code implementation and the review of the Code relevance and effectiveness need to be updated?
No
[Q17x4]
Please comment on the WHO health workforce support and safeguards list (e.g. if your country is included in the list, how has that affected you; if your country is reliant on international health personnel, how has the list affected you; if your country is not in the list, how has it affected you)
[Q18]
Submit any other complementary comments or material you may wish to provide regarding the international recruitment and migration of health personnel, as related to implementation of the Code.
Please describe OR Upload (Maximum file size 10 MB)
Please describe OR Upload (Maximum file size 10 MB)
[Q18x1]
Warning
[INFOxNRI16]
National Reporting instrument 2024
[WARN]
You have reached the end of the National Reporting Instrument - 2024. You may go back to any question to update your answers or confirm your entry by clicking ‘Submit’.